Head and neck
Vol. 45: 111TH CONGRESS SIOECHCF - OFFICIAL REPORT 2025
Surgical margins after open versus transoral surgery for oropharyngeal cancer and their impact on the need for multimodal treatments
Abstract
Objective. In oropharyngeal squamous cell carcinoma (OPSCC), proper definition of surgical margins may have substantial impact on oncologic outcomes. Minimally-invasive techniques prioritise reduced morbidity, yet open approaches remain significant due to limited large-scale evidence comparing their outcomes with transoral methods. The purpose of the present systematic review was to assess the incidence of positive margins in OPSCC management based on surgical approach (open vs transoral) and the subsequent risk of additional treatments.
Methods. Medical databases were searched including PubMed, Scopus, EMBASE, and Cochrane Library from January 2000 to August 2024. Data analysis was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis, and the quality of studies was evaluated using the Newcastle-Ottawa Scale.
Results. Four studies, including 305 patients (126 treated by an open approach, and 179 by transoral surgery), were qualitatively analysed. No significant difference was found in the rates of positive margins (p = 0.422) or need for adjuvant therapy (p = 0.368) between the two approaches. It was not feasible to conduct a meta-analysis due to significant inconsistencies in the reporting of data across the studies included.
Conclusions. Transoral approach is recommended for early-stage OPSCC when adequate exposure is achievable, although its impact on positive surgical margins remains unclear. The management of close or positive margins remains debated due to the oropharyngeal unique anatomy and function, with no clear de-intensification protocol established.
Introduction
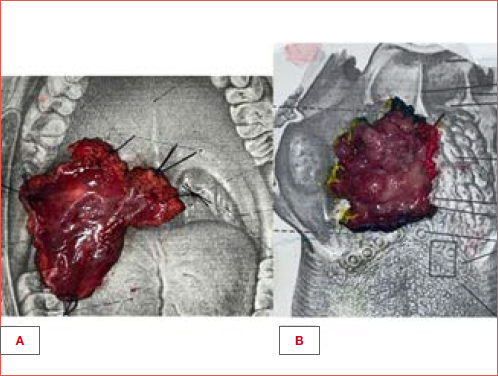
Over the past decades, management of head and neck cancer has undergone a paradigm shift, transitioning from open, invasive surgical approaches to techniques that prioritise organ function preservation. This evolution is particularly evident in the treatment protocols for oropharyngeal squamous cell carcinoma (OPSCC), driven by advancements in oncological understanding and surgical technologies. The more favourable prognosis of human papilloma virus (HPV)-related OPSCC and the ongoing development of minimally-invasive surgical techniques pursue the ambitious goal of achieving oncological radicality while preserving function 1-3. Traditional surgical approaches to OPSCC, such as mandibulotomy, lingual release, or pharyngotomy, often require extensive demolitions to access and remove the primary tumour 4. These open techniques involve significant morbidity, including the need for free tissue transfer and tracheostomy to restore organ function and preserve upper airway competence 5. Consequently, the upfront use of open surgery for primary oropharyngeal tumours has declined, as studies have shown that non-surgical options, such as definitive chemoradiotherapy (CRT) or radiotherapy (RT) alone, can achieve similar loco-regional control and survival outcomes 6,7. However, severe long-term (C)RT morbidities (including osteoradionecrosis, soft tissue fibrosis, neutropenia, dermatitis, xerostomia, and dysphagia) have driven the search for viable alternatives to reduce treatment-related toxicities 8. The development of minimally-invasive techniques, particularly transoral robotic surgery (TORS) and transoral laser microsurgery (TOLMS), has renewed interest in the surgical management of OPSCCs, especially for HPV-positive cases (Cover figure) 9,10. More recently, the adoption of 3D exoscopes has gained attention for their ability to provide excellent visualisation at relatively low costs 11. However, the literature remains controversial regarding the superiority of transoral strategies in terms of surgical and oncological outcomes 12-14. The issue of positive surgical margins in OPSCC surgery plays a pivotal role in this ongoing debate 15. Transoral resections present unique challenges for margins assessment due to piecemeal excision, cautery effects, and tissue retraction 16. Additionally, HPV status further complicates the discussion on the true benefits of adjuvant treatments in young patients with early-stage p16-positive OPSCC and positive surgical margins 17,18. Although current guidelines recommend adjuvant CRT for patients with involved margins 19, the decision-making process must carefully balance effective oncologic control with preserving function and minimising the need for further treatments. The main aim of this systematic review was to evaluate the incidence of positive margins in OPSCC depending on the surgical approach (open vs transoral), as well as their subsequent risk of requiring adjuvant treatments. Furthermore, functional and oncologic outcomes, along with the risk of complications, have been evaluated as secondary outcomes.
Materials and methods
Search strategy and eligibility criteria
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. No ethical approval nor informed consent were required for this study since all reported data were obtained from published literature.
The inclusion criteria for studies selection were chosen according to the PICOS tool: Patients (P), adults affected by OPSCC; Intervention (I), open surgical approach; Comparator (C), transoral surgical approach; Outcomes (O), surgical margin status based on operative approach and their impact on the need of further treatments (primary outcomes) and on functional outcomes, survival, and risk of complications (secondary outcomes); Study design (S), retrospective and prospective cohort studies. The inclusion criteria were: (1) patients affected by OPSCC confirmed by histopathology; (2) comparison between patients undergoing open versus transoral surgical approach with no history of previous treatments; (3) margins reported as clear or close/positive, with definition of the categories included in the paper; (4) margins status and correlation with the type of surgical approach chosen and the ensuing need for adjuvant treatment(s) (RT, CT or CRT).
The exclusion criteria were as follows: (1) articles in a language other than English; (2) full-text form not available; (3) articles which reported insufficient data or from which data were not extractable; (4) analysis of different head and neck malignancies or SCC derived from other sites; (5) previously treated patients; (6) book chapters, letters to the editor, poster presentation, and case reports.
We performed a systematic search of articles published from January 2000 until August 2024 in PubMed, Cochrane Library, EMBASE, and Scopus databases with the combined query: (“oropharynx” OR “oropharyngeal”) AND (“surgical margins”). The full text of relevant studies was screened for final selection. References of all studies included were reviewed to identify any other potentially eligible study.
Data collection
The literature search was conducted independently by two investigators (MVV and PC). Records identified through database searching were merged and duplicates removed. All articles were initially screened for relevance by title and abstract. Studies that met the established criteria were downloaded and their full texts reviewed to determine eligibility. Systematic data extraction from the included studies was made using a structured form, and data were archived in a customised Excel® (Microsoft Corp, Seattle, WA) spreadsheet. Two authors (MVV and PC) independently compiled a standardised form to extract the following information from the included studies: year of publication, study design, total number of patients, subsite of primary, patient demographics, tumour staging, criteria in choice of treatment, surgical approach (open vs transoral), neck management, margin descriptions, adjuvant treatment, HPV status, complications rate, survival, and functional outcomes.
Risk of bias and study quality assessment
Following data collection, we independently assessed the quality of each study in accordance with the Newcastle-Ottawa Scale (NOS)20,21, a scoring system that evaluates potential studies in terms of participants selection, comparability of study groups, and outcomes. Studies are graded one point each for all items except comparability which has the potential to score up to 2 points. Every single study was given a total score ranging from 0 to 9, with scores equal to or greater than 7 considered high quality and scores less than 7 considered low quality. Moreover, a funnel plot was created using the effect size of each primary outcome to examine a potential publication bias.
Results
Data sources
The research selection process is presented in the PRISMA flow diagram shown in Figure 1. At first, 1148 records were found through database searches and identified an additional 2 publications within the reference list of, or citing, the initially selected articles. Out of the 754 articles that remained after duplicates were removed and prescreening was completed, 692 publications were excluded because of irrelevance of the topic through title and abstract screening. Specific inclusion and exclusion criteria, as outlined above, were applied to the full texts of 59 articles. Of the latter, 4 publications met the full set of criteria and were analysed in this review 5,22-24.
Despite our efforts to conduct a meta-analysis, this was not feasible due to significant inconsistencies in the reporting of data across the included studies. Specifically, several papers lacked essential statistical information, such as confidence intervals, odds or hazard ratios, which are critical for performing a quantitative synthesis. The absence of these measures prevented the reliable pooling of results, necessitating a systematic review instead of a meta-analysis.
Demographics and summary of studies
Basic information for the 4 studies included in the analysis are summarised in Table I, including year of publication, first author, type of study analysis, number of patients which underwent open or transoral surgery. A total of 305 patients were included in 4 studies, 3 retrospective and one prospective, including 126 patients undergoing open surgery and 179 treated by transoral surgery.
In these studies, there were no significant differences in terms of gender and age (Tab. II). All 4 articles considered HPV or p16 status; however, patients were not categorised by type of surgical procedure (open vs transoral), making it impossible to identify any correlation. It should be noted that in Tirelli et al. 5 all patients were HPV-negative, whereas in the other studies (Molony et al. 22, Lee et al. 23, and Ford et al. 24), there was a high incidence of HPV-positive patients: 52%, 68%, and 73%, respectively.
All articles described tumour subsites: there were 229 patients with tonsillar or lateral wall tumours, 60 with tumours of the base of tongue or vallecula, and 8 with soft palate tumours. In one study, subsites were not categorised by type of surgical procedure 22. There was no significant difference (p = 0.823) between the technique used and the tumour subsite.
T and N classification
TN staging was included in most studies (3 of 4). However, in the study by Molony et al. 22 TN staging was not available because it was categorised by p16+ status rather than by surgical procedure.
Considering the remaining 3 articles, there was a significant difference (p = 0.024) between the technique used and the T classification. Specifically, for T1 tumours, the transoral technique was used in 63% of cases, while for T2, T3, and T4 tumours, the open technique was applied in 51%, 60%, and 78% of cases, respectively.
There was no significant difference (p = 0.672) between the technique used and the N classification. Neck dissection was performed almost every time during surgery. In one case 22, there were no details regarding the type of surgery and neck dissection. In the other studies, 112 neck dissections (uni- or bilateral) were carried out in the open surgical approach group, while 119 neck dissections were performed in the transoral group.
Surgical techniques
There was a significant difference (p < 0.001) in the use of the two techniques evaluated. Specifically, the studies by Molony et al. 22 and Lee et al. 23 used the transoral approach in 91% and 75% of cases, respectively, while Tirelli et al.5 used the open approach in 67% of cases. In contrast, the study by Ford et al.24 had an equal number of patients operated on using both techniques. Three of 4 studies, with the exception of Molony et al.22, specified how they selected patients for the transoral vs open approach based on specific criteria. Tirelli et al. 5 matched each patient in a TOLMS cohort with one from a transmandibular surgery cohort and one from a lateral pharyngotomy cohort, based on T category, oropharyngeal subsite, and HPV status. Lee et al. 23 selected patients based on tumour extension and exposure, while Ford et al. 24 classified them according to the TNM stage, including open surgeries performed before TORS was introduced at their institution. Tirelli et al. 5 presented 21 patients in the transoral approach group who underwent TOLMS, while the open approach group included 21 patients each undergoing transmandibular surgery and lateral pharyngotomy. In contrast, Molony et al. 22 employed various techniques, with most patients having transoral excision of the primary tumour using monopolar electrocautery without magnification. Eleven patients underwent formal transoral lateral oropharyngectomy, 4 had transoral CO2 laser microsurgery with microscope magnification, and 5 received open surgery via a mandibulotomy approach. In the study by Lee et al. 23the transoral group included 27 patients who underwent TORS, 16 who received radical tonsillectomy via a transoral approach, and 14 who had their primary lesions removed using a transmandibular approach. Ford et al. 24 reported on 65 patients who underwent TORS in the transoral group, while the open approach included transcervical, transfacial, transmandibular, and non-robotic transoral procedures. Normally, we would exclude non-robotic transoral approaches from the open group. However, in this case, the lack of specific information regarding the number of patients treated with transoral resection in the open group makes it negligible. Therefore, we decided to include this study given the diverse range of open surgical techniques considered.
Margin status and surgical procedure
Most studies included defined margin status similarly. Clear margins were consistently defined as > 5 mm, close (when described) was defined as either ink at 5 mm or 1-5 mm, and involved was determined as either < 1 mm or involvement at ink 15,25,26. Because not all articles defined margins as close, but only as positive or negative, in our analysis we decided to consider close margins as negative margins. Overall, 29 of 126 (23%) margins resulted positive in the open surgery group and 37 of 179 (20.7%) were positive in the transoral group (Tab. III). Using the data from the studies and assessing the heterogeneity, a fixed-effects estimate was chosen. The output indicates that there was no heterogeneity (I2 = 10.55%, fixed model p = 0.340). A funnel plot was created to examine a potential publication bias (Fig. 2).
Finally, there was no difference in the surgical approach used between positive and negative margins (p = 0.422). Given the surgical technique used, categorising margin positivity or negativity by subsites, HPV status, or T category was not feasible in any of the articles included in this review.
Adjuvant treatment(s) and surgical procedure
Out of 4 publications included in our analysis, only 3 provided information on adjuvant treatment(s), typically described as RT, CT, or CRT (Tab. IV). The administration of adjuvant therapy was based on internationally recognised indications, such as perineural or lympho-vascular spread, positive margins, or residual tumour 19,25. However, not all articles specified the type of adjuvant treatment(s) administered, nor was it explicitly stated how many patients who underwent CRT also had positive surgical margins. For example, in the study by Lee et al. 23 it is only mentioned whether or not patients received adjuvant treatment, without further details. Furthermore, in Molony et al. 22 cohort, adjuvant treatment information was not available because the need for RT or CRT was categorised by p16+ status rather than by surgical procedure.
Using the data from the studies and assessing heterogeneity, a fixed-effects estimate was chosen. The output indicated that there is no significant heterogeneity (I2 = 55.36%, fixed model p = 0.106). A funnel plot was created to examine a potential publication bias (Fig. 3).
There was no difference in the surgical approach between patients who received adjuvant therapy and those who did not (p = 0.368).
Risk of complications
Among the 4 articles reviewed, only 2 provided details on complications related to the treatment. Tirelli et al. 5 reported complication rates (33.3% for transoral surgery, 47.6% for transmandibular surgery, and 23.8% for lateral pharyngotomy) without specifying the exact issues. On the other hand, Lee et al. 23 offered more insight, noting no complications after transoral surgery but observing osteoradionecrosis and malunion in 2 patients who underwent a mandibulotomy approach.
Survival and functional outcomes
All studies exhibited significant heterogeneity regarding survival and functional outcomes in relation to margins and surgical approach. Only one study 23 reported the 5-year overall survival (OS) rate, and 2 studies 5,23 provided data on 2-year disease-free survival (DFS). The remaining studies did not offer information relevant to our analysis. Indeed, it was not possible to perform an analysis on survival outcomes in this review due to the lack of consistent data. At the same time, a similar issue was found with functional outcomes, as only 2 studies (Lee et al. 23 and Tirelli et al. 5) addressed this aspect.
Discussion
Although several meta-analyses and reviews 12-14 have recently been published on surgical techniques for OPSCC treatment, to our knowledge, this is the first systematic review to address the critical issue of positive surgical margins by comparing open and transoral approaches. Positive margins remain a significant concern, as patients who undergo upfront surgical strategies and subsequently have positive margins are more likely to require adjuvant CRT, regardless of their HPV status 14,27-29. While the primary goal of surgical resection is to minimise or avoid adjuvant treatment(s), positive margins may paradoxically increase the overall treatment burden 19,30. Surprisingly, despite the topic significant implications, only 4 studies, involving just 305 patients over a 20-year period, met the inclusion criteria for our review 5,22-24. This limited research base likely reflects the challenges of creating homogeneous patient groups with consistent oncologic criteria, particularly in centres with established expertise in both transoral and open surgical techniques. Moreover, ethical considerations surrounding randomising surgical approaches, which often depend on tumour-specific characteristics, add complexity to the research landscape.
The key finding of our review showed the rate of positive surgical margins was approximately 20%, regardless of the surgical approach. The surgical technique (open vs transoral) was primarily influenced by tumour extent and ease of exposure. Notably, transoral techniques were used in 63% of early-stage T1-T2 tumours, regardless of anatomical subsite. In less than 40% of T1-T2 cases an open approach was employed primarily due to the challenging tumour exposure, though a small portion of patients were addressed to open surgery because transoral techniques had not yet been introduced at their institution 24. In a different attempt, Chen et al. 13 conducted a meta-analysis of 7 studies comparing TORS and non-robotic surgeries (both transoral non-robotic and open approaches) for OPSCC, finding no clear advantage for one technique over the other, in terms of functional and oncologic outcomes, including positive margins. Similarly to our systematic review, patients undergoing TORS were typically characterised by lower T-category tumours. Additionally, a meta-analysis by Park et al. 12 reported that TORS yielded a lower rate of positive margins compared to open surgery, although the difference was not statistically significant. The comparable rate of positive surgical margins between open and transoral approaches suggests the advantage of choosing the less invasive option. Notably, in transoral surgery positive margins carry a different significance compared to an open technique: one of the key benefits of minimally-invasive techniques is the ability to address positive margins through reoperation, thereby minimising their impact while avoiding significant additional morbidity. Moreover, positive margins can often result from challenges in pathological assessment, such as specimen tearing 31, piecemeal tumour resection, the effect of electrocautery near the tumour edges, or shrinkage of the resected tissue 16. These factors may result in close or positive margins on the pathology report, even when the tumour has been fully resected. Indeed, some studies have shown that positive surgical margins do not always negatively affect OS 27,28. Han et al. 27 demonstrated that among patients treated with surgery alone, positive surgical margins did not significantly affect OS. Additionally, the meta-analysis by Gorphe et al. 28 found no significant difference in local control between 48 patients with close margins and 249 with clear margins (p = 0.249) treated with transoral conventional surgery, TOLMS, and TORS.
Surgical margin status in OPSCC is typically classified according to the histological surgical distance (SD) from the tumour margin, with categories defined as involved (< 1 mm), close (1-5 mm), and clear (> 5 mm) 15,25,26,32. Nevertheless, determining adequate surgical margins in OPSCC requires a thorough assessment of multiple factors 15. First and foremost, since the oropharyngeal wall is typically less than 5 mm thick, some authors proposed that SD in OPSCC could be reduced accordingly 15,33. Anatomical constraints can limit the surgeon’s ability to achieve sufficient deep margins, depending on the specific boundaries of the primary tumour 15,34. For instance, in tumours of the tonsillar fossa, deep margins are limited by the parapharyngeal space, which does not exceed the thickness of the superior constrictor muscles. In contrast, tumours at the base of the tongue have no deep muscular boundaries, and margins here are expected to be at least as wide as those for the oral tongue. According to Persky et al. 35base of the tongue tumours are more likely to show positive deep margins after transoral resection than palatine tonsil tumours. In our systematic review, the scarcity and heterogeneity of data did not allow us to assess positive margins in relation to specific subsites within the oropharynx. In the same way, it was not possible to compare the effectiveness, in terms of surgical margins, of the latest transoral technologies such as TORS, TOLMS, endoscopes, surgical loupes, different types of lasers, and electrocautery devices.
The recent literature highlights that new technologies in minimally-invasive approaches can play a crucial role in determination of surgical margins. For example, Benazzo et al. 16,36 demonstrated that laser technology causes less thermal damage than monopolar electrocautery, reducing the risk of false positive surgical margins. Additionally, Crosetti et al. 11 reported that the use of the exoscope offers an additional advantage by combining enhanced magnified visualisation of tumour margins with the ability to palpate the tumour, unlike TORS.
In our review, it was not possible to make a comparison regarding the type of treatment, the T category, or oncological and functional survival data, particularly in the context of adjuvant therapy. In the selected studies, a total of 85% of patients underwent adjuvant therapy regardless of the surgical technique used, with only 20% of them being justified by the presence of positive margins. This suggests that other factors, such as extracapsular extension, perineural invasion or lympho-vascular spread may also play an important role. Findings from the EORTC 22931 trial 37 showed an OS benefit for CRT in OPSCC with positive surgical margins. Furthermore, Fenlon et al. 17 in 2021 reported no positive effect on OS of adjuvant CRT compared to adjuvant RT alone in p16-positive OPSCC patients with positive surgical margins. In a similar effort, Skillington et al. 38 showed that among patients with p16-positive OPSCC managed surgically with adjuvant RT, the addition of chemotherapy provided no additional benefit in terms of DFS and was associated with worse OS. On the other hand, Park et al. 39 found that in T1-T2 lesions without other risk factors, even with a safety margin of ≥ 1 mm, adjuvant therapy can potentially be omitted.
There are several limitations to this systematic literature review. First and foremost, the articles considered are few, involve small cohorts and are mostly retrospective in nature. Each study followed different criteria regarding the choice between transoral and open surgery, leading to variability across centres. All 4 studies reported HPV or p16 status, but patients were not categorised by the surgical approach (open or transoral), limiting the ability to correlate HPV status with oncological outcomes or determine if one technique is the most effective based on HPV status. Finally, we made the deliberate decision to exclude articles involving cohorts of patients undergoing salvage surgery, as the anatomy and tumour extent in recurrent cases differ fundamentally from those in primary tumours.
Conclusions
When managing early-stage OPSCC, a transoral approach should be recommended as the first-line treatment, provided that exposure conditions are favourable. The impact of the latest technologies on margin positivity remains undefined. Indeed, the management of close and positive margins continues to be a subject of debate, given the unique anatomical and functional characteristics of the oropharyngeal region. Although positive margins pose a significant challenge, the lack of robust data prevents the establishment of a clear de-intensification protocol for adjuvant treatment, even in HPV-positive patients. Lastly, the scarcity of high-quality literature, coupled with the predominance of retrospective studies, highlights the urgent need for prospective and multicentre studies to better understand and optimise the management of positive surgical margins.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors contributed to the interpretation of the data, critically revised the manuscript for important intellectual content, and approved the final version of the manuscript.
Ethical consideration
Not applicable.
History
Received: February 4, 2025
Accepted: March 10, 2025
Figures and tables
Figure 1. The research selection process is presented in the PRISMA flow diagram.
Figure 2. Funnel plot examining potential publication bias in papers on surgical margins according to open vs transoral approach.
Figure 3. Funnel plot examining potential publication bias in papers on adjuvant treatment(s) according to different surgical approaches.
| Author | Year | Type of analysis | Number of patients | Criteria in choice of treatment | NOS score | |
|---|---|---|---|---|---|---|
| Open surgery | Transoral surgery | |||||
| Lee et al. 23 | 2013 | Prospective | 14 | 43 | Extension of disease, exposure | ≥ 7 |
| Ford et al. 24 | 2014 | Retrospective | 65 | 65 | TNM stage | ≥ 7 |
| Molony et al. 22 | 2017 | Retrospective | 5 | 50 | N/A | ≥ 7 |
| Tirelli et al. 5 | 2021 | Retrospective | 42 | 21 | T stage, oropharyngeal subsite, HPV status | ≥ 7 |
| TORS: transoral robotic surgery; HPV: human papilloma virus; N/A: not available; NOS: Newcastle-Ottawa Scale. | ||||||
| Characteristics | Lee et al. 23 | Ford et al. 24 | Molony et al. 22 | Tirelli et al. 5 | ||||
|---|---|---|---|---|---|---|---|---|
| Open | Transoral | Open | Transoral | Open | Transoral | Open | Transoral | |
| Mean age | 57.9 | 58.5 | 54.9 | 63.2 | ||||
| Gender | ||||||||
| Female | 11 | 27 | 11 | 12 | ||||
| Male | 46 | 103 | 44 | 51 | ||||
| HPV /p16 status | ||||||||
| Positive | 39 | 95 | 29 | 0 | ||||
| Negative | 18 | 35 | 26 | 63 | ||||
| Subsites | ||||||||
| Tonsils/lateral wall | 14 (24.6%) | 43 (75.4%) | 55 (42.3%) | 44 (33.8%) | 40 (72.7%) | 22 (34.9%) | 11 (17.5%) | |
| BOT/vallecula | 0 | 0 | 9 (6.9%) | 21 (16.2%) | 8 (14.6%) | 20 (31.7%) | 10 (15.9%) | |
| Soft palate | 0 | 0 | 1 (0.8%) | 0 | 7 (12.7%) | 0 | 0 | |
| T classification | ||||||||
| T1 | 0 | 16 (28%) | 21 (16.2%) | 21 (16.2%) | NA | 4 (6.3%) | 5 (7.9%) | |
| T2 | 11 (19.3%) | 21 (36.8%) | 36 (27.7%) | 36 (27.7%) | 20 (31.7%) | 7 (11.1%) | ||
| T3 | 3 (5.3%) | 6 (10.5%) | 6 (4.6%) | 6 (4.6%) | 23 (36.5%) | 9 (14.3%) | ||
| T4 | 0 | 0 | 2 (1.5%) | 2 (1.5%) | 5 (7.9%) | 0 | ||
| N classification | ||||||||
| N+ | NA | 51 (39.2%) | 51 (39.2%) | NA | 27 (42.9%) | 14 (22.2%) | ||
| N0 | 14 (10.8%) | 14 (10.8%) | 15 (23.8%) | 7 (11.1%) | ||||
| HPV: human papilloma virus; BOT: base of tongue. | ||||||||
| Study | Open approach | Transoral approach | ||||
|---|---|---|---|---|---|---|
| Positive | Negative | % positive | Positive | Negative | % positive | |
| Lee et al. 23 | 1/14 | 13/14 | 7.1 | 3/43 | 40/43 | 7 |
| Ford et al. 24 | 10/65 | 55/65 | 15.4 | 12/65 | 53/65 | 18.5 |
| Molony et al. 22 | 2/5 | 3/5 | 40 | 19/50 | 31/50 | 90.5 |
| Tirelli et al. 5 | 16/42 | 26/42 | 38 | 3/21 | 18/21 | 14.3 |
| Total | 29/126 | 97/126 | 23% | 37/179 | 142/179 | 20.7% |
| Study | Open approach | Transoral approach | ||||
|---|---|---|---|---|---|---|
| Surgery alone | Surgery + adjuvant treatment | % Adjuvant treatment | Surgery alone | Surgery+ adjuvant treatment | % Adjuvant treatment | |
| Lee et al. 23 | 3/14 | 11/14 | 78.6 | 6/43 | 36/43 | 85.7 |
| Ford et al. 24 | 6/65 | 59/65 | 90.8 | 5/65 | 60/65 | 92.3 |
| Tirelli et al. 5 | 7/42 | 35/42 | 83.3 | 9/21 | 12/21 | 57.1 |
| Total | 16 | 105 | 86.8% | 20 | 108 | 84.4% |
References
- Costantino A, Magnuson JS, Alamoudi U, et al. Prognostic significance of Human Papillomavirus genotypes in oropharyngeal squamous cell carcinoma. Laryngoscope 2025;135:695-704. https://doi.org/10.1002/lary.31775
- Ceremsak J, Ye W, Hicks M, et al. Treatment de-escalation in oropharyngeal carcinoma and the role of robotic surgery. Surg Oncol Clin N Am 2024;33:697-709. https://doi.org/10.1016/j.soc.2024.07.001
- Molteni G, Bassani S, Arsie AE, et al. Role of TORS as de-escalation strategy in HPV-related oropharyngeal cancer, what we need to know. Healthcare (Basel) 2024;12:1014. https://doi.org/10.3390/healthcare12101014
- Almeida Parra F, Bueno De Vicente Á, Ranz Colio Á, et al. Transmandibular approach in head and neck oncological surgery. Chin J Dent Res 2020;23:257-264. https://doi.org/10.3290/j.cjdr.b867885
- Tirelli G, Bertolin A, Guida F, et al. Post-operative outcomes of different surgical approaches to oropharyngeal squamous cell cancer: a case-matched study. J Laryngol Otol 2021;135:348-354. https://doi.org/10.1017/S0022215121000876
- Thakar A, Panda S, Kakkar A, et al. A matched pair analysis of oncological outcomes in human papillomavirus-negative oropharyngeal squamous cell carcinoma: transoral surgery versus radiotherapy or concurrent chemoradiation. Head Neck 2021;43:2896-2906. https://doi.org/10.1002/hed.26771
- Pedro C, Mira B, Silva P, et al. Surgery vs primary radiotherapy in early-stage oropharyngeal cancer. Clin Transl Radiat Oncol 2017;9:18-22. https://doi.org/10.1016/j.ctro.2017.12.002
- Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, et al. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 2008;26:3770-3776. https://doi.org/10.1200/JCO.2007.14.6647
- Golusiński W, Golusińska-Kardach E. Current role of surgery in the management of oropharyngeal cancer. Front Oncol 2019;9:388. https://doi.org/10.3389/fonc.2019.00388
- Ferris RL, Flamand Y, Weinstein GS, et al. Phase II randomized trial of transoral surgery and low-dose intensity modulated radiation therapy in resectable p16+ locally advanced oropharynx cancer: an ECOG-ACRIN Cancer Research Group Trial (E3311). J Clin Oncol 2022;40:138-149. https://doi.org/10.1200/JCO.21.01752
- Crosetti E, Arrigoni G, Manca A, et al. 3D exoscopic surgery (3Des) for transoral oropharyngectomy. Front Oncol 2020;10:16. https://doi.org/10.3389/fonc.2020.00016
- Park DA, Lee MJ, Kim SH, et al. Comparative safety and effectiveness of transoral robotic surgery versus open surgery for oropharyngeal cancer: a systematic review and meta-analysis. Eur J Surg Oncol 2020;46:644-649. https://doi.org/10.1016/j.ejso.2019.09.185
- Chen H, Liu Y, Huang D, et al. Transoral robotic surgery vs. non-robotic surgeries for oropharyngeal squamous cell carcinoma: systematic review and meta-analysis. J Robot Surg 2023;17:2537-2546. https://doi.org/10.1007/s11701-023-01689-6
- Groysman M, Gleadhill C, Baker A, et al. Comparison of margins and survival between transoral robotic surgery (TORS) and non-robotic endoscopic surgery for oropharyngeal cancer. Am J Otolaryngol 2023;44:103982. https://doi.org/10.1016/j.amjoto.2023.103982
- Chen Y, Zhong NN, Cao LM, et al. Surgical margins in head and neck squamous cell carcinoma: a narrative review. Int J Surg 2024;110:3680-3700. https://doi.org/10.1097/JS9.0000000000001306
- Benazzo M, Canzi P, Mauramati S, et al. Transoral robot-assisted surgery in supraglottic and oropharyngeal squamous cell carcinoma: laser versus monopolar electrocautery. J Clin Med 2019;8:2166. https://doi.org/ 10.3390/jcm8122166.
- Fenlon JB, Hutten RJ, Weil CR, et al. Comparing adjuvant radiation to adjuvant chemoradiation in postsurgical p16+ oropharyngeal carcinoma patients with extranodal extension or positive margins. Head Neck 2022;44:606-614. https://doi.org/10.1002/hed.26951
- Lechner M, Liu J, Masterson L, et al. HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol 2022;19:306-327. https://doi.org/10.1038/s41571-022-00603-7
- National Comprehensive Cancer Network NCCN Guidelines. Head and Neck Cancer. Available online: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf
- Wells GA, Shea B, Peterson J, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-605. https://doi.org/10.1007/s10654-010-9491-z
- Molony P, Kharytaniuk N, Boyle S, et al. Impact of positive margins on outcomes of oropharyngeal squamous cell carcinoma according to p16 status. Head Neck 2017;39:1680-1688. https://doi.org/10.1002/hed.24824
- Lee SY, Park YM, Byeon HK, et al. Comparison of oncologic and functional outcomes after transoral robotic lateral oropharyngectomy versus conventional surgery for T1 to T3 tonsillar cancer. Head Neck 2014;36:1138-1145. https://doi.org/10.1002/hed.23424
- Ford SE, Brandwein-Gensler M, Carroll WR, et al. Transoral robotic versus open surgical approaches to oropharyngeal squamous cell carcinoma by human papillomavirus status. Otolaryngol Head Neck Surg 2014;151:606-611. https://doi.org/10.1177/0194599814542939
- Colevas AD, Yom SS, Pfister DG, et al. NCCN Guidelines Insights: Head and Neck Cancers, Version 1.2018. J Natl Compr Canc Netw 2018;16:479-490. https://doi.org/10.6004/jnccn.2018.0026
- Woolgar JA, Triantafyllou A. A histopathological appraisal of surgical margins in oral and oropharyngeal cancer resection specimens. Oral Oncol 2005;41:1034-1043. https://doi.org/10.1016/j.oraloncology.2005.06.008
- Han M, Stanford-Moore GB, Larson AR, et al. Predictors of mortality in HPV-associated oropharynx carcinoma treated with surgery alone. Laryngoscope 2020;130:E423-E435. https://doi.org/10.1002/lary.28344
- Gorphe P, Simon C. A systematic review and meta-analysis of margins in transoral surgery for oropharyngeal carcinoma. Oral Oncol 2019;98:69-77. https://doi.org/10.1016/j.oraloncology.2019.09.017
- Holcomb AJ, Herberg M, Strohl M, et al. Impact of surgical margins on local control in patients undergoing single-modality transoral robotic surgery for HPV-related oropharyngeal squamous cell carcinoma. Head Neck 2021;43:2434-2444. https://doi.org/10.1002/hed.26708
- Maniaci A, Hao SP, Cancemi F, et al. Surgical treatment for advanced oropharyngeal cancer: a narrative review. Medicina (Kaunas) 2023;59:304. https://doi.org/10.3390/medicina59020304
- Mistry RC, Qureshi SS, Kumaran C. Post-resection mucosal margin shrinkage in oral cancer: quantification and significance. J Surg Oncol 2005;91:131-133. https://doi.org/10.1002/jso.20285
- Brinkman D, Callanan D, Jawad H, et al. Comparison of Royal College of Pathologists and College of American Pathologists definition for positive margins in oral cavity squamous cell carcinoma. Oral Oncol 2022;127:105797. https://doi.org/10.1016/j.oraloncology.2022.105797
- Tomblinson CM, Fletcher GP, Hu LS, et al. Determination of posterolateral oropharyngeal wall thickness and the potential implications for transoral surgical margins in tonsil cancer. Head Neck 2021;43:2185-2192. https://doi.org/10.1002/hed.26693
- Hinni ML, Ferlito A, Brandwein-Gensler MS, et al. Surgical margins in head and neck cancer: a contemporary review. Head Neck 2013;35:1362-1370. https://doi.org/10.1002/hed.23110
- Persky MJ, Albergotti WG, Rath TJ, et al. Positive margins by oropharyngeal subsite in transoral robotic surgery for T1/T2 squamous cell carcinoma. Otolaryngol Head Neck Surg 2018;158:660-666. https://doi.org/10.1177/0194599817742852
- Benazzo M, Canzi P, Occhini A. Transoral robotic surgery with laser for head and neck cancers: a feasibility study. ORL 2012;74:124-128. https://doi.org/10.1159/000337092
- Bernier J, Cooper JS, Pajak TF, et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (#9501). Head Neck 2005;27:843-850. https://doi.org/10.1002/hed.20279
- Skillington SA, Kallogjeri D, Lewis JS Jr, et al. The role of adjuvant chemotherapy in surgically managed, p16-positive oropharyngeal squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg 2017;143:253-259. https://doi.org/10.1001/jamaoto.2016.3353
- Park YM, Lim JY, Koh YW, et al. Surgical margin status and role of adjuvant therapy in human papillomavirus-positive oropharyngeal cancer. Head Neck 2023;45:2369-2376. https://doi.org/10.1002/hed.27473
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 796 times
- PDF downloaded - 224 times



