Laryngology
Vol. 45: Issue 6 - December 2025
Italian multicentre study to validate the Swallowing Outcome After Laryngectomy (SOAL) questionnaire
Abstract
Objective. To report the data obtained by translating the Swallowing Outcomes After Laryngectomy (SOAL) questionnaire in Italian to validate it and offer a valid tool for Italian-speaking patients and clinicians.
Methods. A multicentre case-control study was performed between January 1st 2024 and October 1st 2024. In all, 494 patients consecutively treated for laryngeal squamous cell carcinoma were included in the study (group 1). Healthy controls and patients who underwent radiotherapy (group 2) or chemotherapy (group 3) of the head and neck district were the two control groups.
Results. Statistically significant differences were observed comparing SOAL scores among the three groups (ANOVA: p < 0.0001); significant differences were observed between group 1 (mean 0.89 +/- 1.31; 95% CI: 0-3) and group 2 (mean 6.78 +/- 4.59; 95% CI: 1-24) (Bonferroni-Holmes [BH] p < 0.01), and group 1 and group 3 (mean 11 +/- 7.47; 95% CI: 0-38) (BH: p 0 < 0.01). Statistically significant differences in the SOAL scores were also identified between group 2 and 3 (BH: p < 0.01).
Conclusions. The SOAL questionnaire may be a useful tool to correctly understand patients’ concerns for swallowing to promptly and rapidly manage them and improve patient’s quality of life.
Introduction
Laryngeal squamous cell carcinoma (LSCC) has an incidence rate of just over 6 cases per 100,000 people per year, with around 13,000 new diagnoses in the United States each year 1,2. Smoking and alcohol use are the two independent and synergistic risk factors that contribute to tumour onset; human papillomavirus (HPV) is occasionally identified in LSCC supporting the concepts that habits (lifestyle factors) impact more than HPV 3-5. Despite improvements in surgery, radiotherapy (RT) and chemotherapy (ChT), survival rates for LSCC have remained unchanged over the years.
The tumour site is relevant to the sequelae. After LSCC removal (whether reconstructive or total laryngectomy, TL) phonation and swallowing can become difficult, which has a significant impact on the patient’s quality of life (QoL).
Phonation prosthesis is an excellent device for restoring vocal function; on the other hand, swallowing problems are difficult for both patients and surgeons to manage. Deficit or alterations in swallowing can be bothersome and sometimes risky. Patients may have difficulty explaining their swallowing difficulties during a clinical consultation, but a patient-reported questionnaire could help to speed up and simplify communication between patients and doctors.
In 2012, Govender et al. developed and validated the Swallowing Outcome After Laryngectomy (SOAL) questionnaire, a 17-item instrument with acceptable psychometric properties to assess swallowing functions after TL 6,7. The SOAL questionnaire is in English; sometimes translation of questionnaires into other languages can be challenging, which reduces the efficacy of the original tool.
The aim of this paper is to report the data obtained by translating the SOAL questionnaire into Italian, in order to validate and provide Italian-speaking patients and clinicians with a useful tool.
Materials and methods
This multicentre case-control study was conducted between January 1st 2024 and October 1st 2024. All patients who were consecutively treated for LSSC and followed by a multidisciplinary oncology group in each of the Otolaryngology departments involved in the study were included.
Translational and cross-cultural adaptation of the SOAL questionnaire was performed using standard techniques 8. The original SOAL questionnaire was translated in Italian by two professional translator and three physicians fluent in English (PDL, FA, ADS). The two translators and committee of the experts combined the results of the translations in an Italian back-translated version, which was compared with the original in English to check that it had the same semantic value. Disagreeing points were resolved, the final version was defined by consensus of all the authors after the review of expert committee, and the definitive questionnaire was pre-tested on 32 subjects. Table I shows the final Italian version of the SOAL questionnaire which was validated in the present study.
Original SOAL questionnaire
The SOAL is a validated 17-item questionnaire. The final version of the translated and adapted questionnaire was administered to patients. It was designed for quick and easy administration in a clinical setting, either by self-administration or by an interviewer. Each item on the questionnaire assesses a single swallowing characteristic:
- Severity: a three-point scale is used to assess the severity of the symptom. The scale (“no”, “a little”, “a lot”) uses the language most commonly employed by patients to describe their issues 6;
- Bothering: The significance of the symptom was assessed by the question ‘Does this symptom bother you?’.
Each severity response was scored: “No” = 0, “a little” = 1, and “a lot” = 2. The scores from the 17 items were summed to give the subject’s SOAL score in the range 0-34, where low scores corresponded to better conditions.
The patients and the control group, to whom the translated SOAL was administered, were divided into three groups:
- Group 1 (healthy controls): healthy people who have not undergone any type of surgery (including radiofrequency) at the level of the pharynx or larynx, never undergone RT of the head and neck region, and who have no known history of major or minor neurological disorders, including head trauma in the 6 months prior to recruitment;
- Group 2: patients who have undergone TL (at least 3 months since the last oncological treatment);
- Group 3: patients with dysphagia who had undergone RT/ChT of the head and neck district (for any type of head and neck cancer), and who were recruited at least 3 months after completing therapy.
The inclusion and exclusion criteria were as described below.
The eligibility criteria were as follows: a previous diagnosis of untreated head and neck cancer and/or previous treatment (RT/ChT) as part of cancer management, no associated neurological disease, and cognitive ability within normal limits (Mini-Mental State Examination > 25, corrected for age and educational level).
The exclusion criteria were: age under 18 years, pregnancy, psychiatric disorders or cognitive impairment (Mini-Mental State Examination < 25, corrected for age and educational level), previous open partial horizontal laryngectomy (OPHL), refusal to participate in the study, and previous/known neurological conditions impacting swallowing or previous laryngeal or pharyngeal surgery.
Food habits were evaluated by asking patients directly. Diet was classified as “normal” if patients could swallow solid, semi-liquid and liquid foods without problems; “modified” if patients presented dysphagia for semi-liquid and liquid foods but not for solid foods, and “no oral intake” if enteral or parenteral food intake was necessary due to severe dysphagia and high risk of aspiration pneumonia.
A score 1 was assigned to normal intake, 2 to modified intake, and 3 to no oral intake; if diet was not classifiable, a score of 4 was assigned. Patients with different diet scores could belong to groups 2 or 3. Patients in the control group always had a normal diet.
There was an opportunity to modify the answers once the SOAL questionnaire had been filled in. In addition to the responses to the questionnaire and dietary information, further information was collected and stored on a computer accessible only to the referent, in order to preserve patients’ privacy and reduce the risk of a data breach. These data included: gender; age at the time of completing the questionnaire; pathological tumour stage (using the 8th edition of the American Joint Committee on Cancer (AJCC)/ Union International Contre le Cancer (UICC) TNM classification); whether or not reconstructive flaps were used and, if so, the type; type of resection; closure technique; number of closure layers; type of myotomy; follow-up time in months; diet; adjuvant treatment (RT alone vs ChT alone vs RTChT). As suggested by Govender et al. 6, we considered a SOAL score of less than 5 to be normal.
Statistical analysis
The percentage was calculated. The numerical data were analysed using a one-way ANOVA and a Bonferroni-Holmes (BH) “ad hoc” test. This test was used to analyse the difference in age between the three groups, and to compare the results obtained by SOAL questionnaire between the three groups. Pearson test was used to analyse the correlation between diet and SOAL scores. In cases where information regarding the diet (see Materials and Methods) was absent, the dietary data and SOAL scores were excluded from statistical analysis. For all tests, a p-value of less than or equal to 0.05 was considered statistically significant. The statistical analyses were performed using Prism 10®.
Results
A total of 494 people were included in the study. Group 1 comprised 165 individuals (71 women [43%] and 94 men [57%]aged 47 ± 18.2 years); Group 2 comprised 152 people (24 women [15.8%] and 128 men [84.2%] aged 68.4 ± 8.9 years); Group 3 comprised the remaining 177 individuals (66 women [37.3%]and 111 men [62.7%] aged 66.4 ± 11.5 years).
Table II shows the demographic characteristics of the three groups and the distribution of diet types between the groups, while Table III shows surgical, pathological and follow-up data.
All patients in Group 1 had a normal diet.
Among patients in Group 2, 113 (74%) had a normal diet, 30 (20%) had a modified diet, and only 2 patients (1%) had no oral intake (data were not available for 7 patients, 5%). Of these patients, 125 (82%) underwent TL for cT3 or cT4a LSCC and 25 underwent TL after RT failure (salvage laryngectomy); the majority of patients in this group did not undergo reconstructive surgery (n = 132, 87%), required surgery to the larynx only (n = 91, 60%), and showed a single layer (n = 98, 65%) horizontal closure (n = 152, 100%). Regarding adjuvant therapy, 47 patients (31%) underwent RT alone, and 38 (25%) underwent RTChT, and 67 subjects (44%) did not require adjuvant treatment.
All patients in Group 3 had previously undergone RTChT in the head and neck district for oncological reasons. Of these patients, 99 (56%) had a normal diet, 51 (29%) had a modified diet, and 14 (8.5%) belonged to the no oral intake subgroup (data were not available for 12 patients, 6.5%).
Statistically significant differences in age were identified among the three groups (ANOVA: p < 0.00001), especially between groups 1 and 2 (BH: p < 0.01) and groups 1 and 3 (BH: p < 0.01). No significant differences were observed comparing the ages of groups 2 and 3 (BH: p > 0.05).
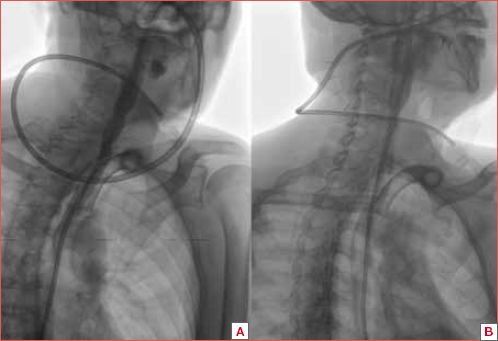
Statistically significant differences in SOAL scores were observed when comparing the three groups (ANOVA: p < 0.0001); specifically, significant differences were observed between Group 1 (average 0.89 + 1.31; CI 95%: 0-3) and Group 2 (mean 6.78 + 4.59; 95% CI: 1-24) (BH: p < 0.01), as well as between Group 1 and Group 3 (mean 11 + 7.47; 95% CI: 0-38) (BH: p < 0.01). Statistically significant differences in the SOAL scores were also identified between groups 2 and 3 (BH: p < 0.01). Figure 1 illustrates the SOAL score comparison between the three groups.
In summary, patients affected by dysphagia following RT had the worst SOAL score. However, SOAL scores of patients who only underwent laryngectomy were better than those who underwent radiotherapy.
We identified a positive, significant correlation between type of diet and SOAL scores (Pearson: p < 0.0001). Since a normal diet was given a score of 1, this result indicates that a higher score, corresponding to modified or altered diets, is directly correlated with the severity of dysphagia, as identified by an increase in SOAL scores.
Discussion
Our results confirm the SOAL questionnaire’s validity as a tool for clinical assessment of swallowing disorders. The Italian version of the questionnaire demonstrated the same ability as the English version to detect the severity of concerns and bothersome sensations. This tool can be used in clinical practice as an efficient, quick and cost-effective method of evaluating swallowing outcomes in patients who previously underwent TL.
TL splits the respiratory (trachea) and swallowing (oesophagus) pathways, swallowing food to be consumed without the risk of inhalation. The main concern of surgeons is therefore the restoration of phonation to improve the patient’s QoL
Over the years, swallowing problems in patients with TL have always been underestimated. Although several questionnaires have been validated to evaluate dysphagia 9,10, before SOAL, there was nothing specific for laryngectomees.
In 2012, Govender et al. described the development and validation of a 17-item SOAL questionnaire 6. Preliminary validation revealed significant differences in SOAL scores between a control group, patients treated by TL, and those treated by RT/ChT 7. Our study, which had the same study design as that of Govender et al. 6, showed overlapping results. These results support and confirm the validity of the Italian version of the SOAL in distinguishing between people with different conditions affecting their ability to swallow.
We also identified a positive correlation between diet and SOAL scores; patients with low SOAL scores (healthy control group) had a normal diet. In contrast, higher SOAL scores were associated with an inability to eat (no oral intake). This confirms that, like its English version, the Italian questionnaire can identify the type of diet based on the increase in scores.
It is important to underline some criticisms in our study, such as the difference in age between the control group and patients.
The control group was notably younger than the other two groups. As swallowing ability can deteriorate with age, even in the absence of overt neurological conditions 11, our results should be carefully considered. While the changes in swallowing are minimal in patients under 75 years of age in the absence of neurological conditions, some differences can be present, for example less than perfect teeth conditions with a negative impact on mastication and oral phase of swallowing. The literature reports an incidence of swallowing disorders in over 65 years between 7% and 22% 12. Moreover, we are currently investigating swallowing function in the elderly (mean age 62.7 years) (unpublished data) compared to those < 50 years and swallowing abilities overlap among the groups. However, additional studies with age-matched participants to determine whether SOAL can detect changes with the same statistically significant value in elderly patients are needed.
The age difference should be considered as one of the limitations of our study, bearing in mind that no more than 10% of healthy people over the age of 65 years present swallowing difficulties 11.
Conversely, there were no differences in age (mean and standard deviation) between groups 2 (laryngectomees) and 3 (patients undergoing head and neck RT).
In accordance with the original study, our volunteers (healthy group) showed the lowest SOAL scores (0.89 +/- 1.31), which were significantly better than those in groups 2 and 3, with mean scores of 6.78 ± 4.59, and 11 ± 7.47, respectively.
Patients treated with RT had the worst scores, which were significantly lower than those of the TL group. This finding can be explained by the well-known adverse outcomes of RT; irradiation of tissues induces mucosal inflammation and adherence between layers, which negatively impacts physiological bolus peristalsis. This, in turn, negatively impacts SOAL severity scores. Furthermore, a metallic taste in the mouth, another common adverse effect of RT, can negatively impact the patient’s perception and increase the “bothering sensation” scores 13.
Examining the results of the SOAL questionnaire exclusively, surgery appears to guarantee better outcomes at least from the patient’s perspective. Based on patient’s feedback, a well-performed surgery with excellent preservation of layers, including plan-by-plan suturing of the muscles and careful skin closure, allows for better outcomes.
A similar concept has previously been discussed in relation to the use of transoral laser microsurgery (TOLMS) for preserving long-term voice outcome compared to RT. This is probably due to the negative effects of the RT on laryngeal tissue, which reduces phonatory capacity.
When considering treatments, it is important to weigh the pros and cons of the available options. In the case of RT, the effect on the mucosa and tissues must be kept in mind. RT has always been considered the best way to preserve organ function: however, thanks to improvements in surgical techniques and the use of robots, it is now possible to minimise the removal of tumour tissue while preserving the laryngeal function. This is a relevant aspect to consider when choosing treatment, particularly for patients with an equivalent survival rate when comparing TOLMS/TL and RT treatment 14,15.
A major limitation of the current study is the absence of analyses of the psychometric properties of the SOAL questionnaire; however, this study design exactly overlaps that of Govender et al. 7 We are currently continuing to screen patients with the Italian version of the questionnaire, in order to collect sufficient data to conduct psychometric evaluations.
Conclusions
The results of our multicentre study confirmed the validity of the Italian translation of the SOAL questionnaire in identifying the severity of dysphagic symptoms and their bothersomeness in patients undergoing treatment for LSCC. Well-performed, surgery seems to be better in terms of swallowing outcomes from the patient’s point of view. The SOAL questionnaire may be a useful tool for understanding patients’ concerns about swallowing and improving their quality of life. Because we did not perform psychometric tests, our results must be considered preliminary; the appropriateness of the Italian version of the questionnaire as a clinical outcome measure must be confirmed by testing its psychometric properties on a larger group of patients.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
PDL, AC: original concept of the studio; PDL, ADS, GP, MF, FA, LG, AVM, NG, TA: manuscript writing, data analysis and validation; PDL, ADS, GP, MF, FA, LG, AVM, NG, TA, LdC, AS, EA, AC: data search; PDL, ADS, FAS, GT, GM, LCa, LuC, RP, LP, MR, AC: reviewing and final approval.
Ethical consideration
Due to the retrospective, non-interventional nature of the study, ethical approval was waived by the local ethics committee in accordance with national and institutional requirements.
The study was conducted in accordance with the Declaration of Helsinki. Prior to surgery, all patients signed a non-specific informed consent form authorising the disclosure of their personal information for scientific purposes. All patients who were alive at the time of the study were informed about it, and none objected to being included.
History
Received: February 22, 2025
Accepted: June 6, 2025
Figures and tables
Figure 1. SOAL score comparison between the three groups.
| No | Un po’ | Molto | Se ha risposto “un pò” o “molto”, ciò la infastidisce? Risponda “sì” o “no” | ||
|---|---|---|---|---|---|
| Q1. Secondo lei, attualmente, ha difficoltà nel deglutire? | . | . | . | No | Sì |
| Q2. Ha difficoltà nel deglutire bevande liquide (tè, acqua, succhi) indipendente dal dislocamento della protesi fonatoria? | . | . | . | No | Sì |
| Q3. Ha difficoltà nel deglutire liquidi più corposi (zuppe, frappé, bevande nutrienti)? | . | . | . | No | Sì |
| Q4. Ha difficoltà nel deglutire cibi morbidi (pasta ben cotta e condita, polpette morbide)? | . | . | . | No | Sì |
| Q5. Ha difficoltà nel deglutire cibi solidi “secchi” (pane, biscotti secchi)? | . | . | . | No | Sì |
| Q6. Quando deglutisce, ha la sensazione che i liquidi le rimangano in gola? | . | . | . | No | Sì |
| Q7. Quando deglutisce, ha la sensazione che i cibi solidi le rimangano in gola? | . | . | . | No | Sì |
| Q8. Quando mangia o beve, il cibo o i liquidi risalgono in bocca o nel naso? | . | . | . | No | Sì |
| Q9. Ha bisogno di assumere liquidi per ingoiare cibi solidi? | . | . | . | No | Sì |
| Q10. Ha bisogno di deglutire più volte a ogni boccone per aiutare il cibo o i liquidi a scendere? | . | . | . | No | Sì |
| Q11. Evita di assumere alcuni cibi perchè non riesce a deglutirli? | . | . | . | No | Sì |
| Q12. Impiega più tempo del normale a consumare un pasto? | . | . | . | No | Sì |
| Q13. Il suo piacere per il cibo si è ridotto? | . | . | . | No | Sì |
| Q14. Ha ridotto la quantità del suo pasto? | . | . | . | No | Sì |
| Q15. Il suo normale appetito si è ridotto perchè non riesce a percepire normalmente l’odore o il sapore del cibo? | . | . | . | No | Sì |
| Q16. Mangiare è diventato più difficile per via di una secchezza orale? | . | . | . | No | Sì |
| Q17. Si sente a disagio a mangiare insieme ad altre persone? | . | . | . | No | Sì |
| Group 1 | Group 2 | Group 3 | p | |
|---|---|---|---|---|
| Sample size (n) | 165 | 152 | 177 | |
| Gender | 71 F, 94 M | 24 F, 128 M | 66 F, 111 M | |
| Mean age ± SD (yr) | 47 ± 18.2 | 68.4 ± 8.9 | 66.4 ± 11.5 | 1 vs 2: p < 0.01 |
| 1 vs 3: p < 0.01 | ||||
| 2 vs 3: p > 0.05 | ||||
| Type of diet | 165 normal diet | 113 normal diet | 99 normal diet | |
| 30 modified | 51 modified | |||
| 2 no oral intake | 15 no oral intake | |||
| 7 no data available | 12 no data available | |||
| SOAL questionnaire score | 0.89 ± 1.31 | 6.78 ± 4.59 | 11 ± 7.47 | 1 vs 2: p < 0.01 |
| 1 vs 3: p < 0.01 | ||||
| 2 vs 3: p < 0.01 |
| Group 2 | Group 3 | |
|---|---|---|
| Sample size (n) | 152 | 177 |
| pT classification | 82 pT3 | / |
| 43 pT4a | ||
| 25 salvage laryngectomy | ||
| 2 no data available | ||
| pN classification | 15 pNx | / |
| 89 pN0 | ||
| 13 pN1 | ||
| 1 pN2a | ||
| 9 pN2b | ||
| 2 pN2c | ||
| 3 pN3a | ||
| 15 pN3b | ||
| Flap reconstruction | 132 primary closure | |
| 5 microvascular free flap | ||
| 15 pectoralis major flap | ||
| Type of resection | 91 larynx alone | |
| 54 pharyngolaryngectomy | ||
| 7 larinx and base of the tongue | ||
| Closure technique | 152 horizontal closure | |
| Layers of closure | 98 single layer | |
| 54 two layers | ||
| Follow-up, months | 41.5 ± 34.7 | |
| Type of adjuvant treatment | 67 TL alone | 177 RTChT |
| 47 RT alone | ||
| 38 RTChT |
References
- Cavaliere M, Bisogno A, Scarpa A. Biomarkers of laryngeal squamous cell carcinoma: a review. Ann Diagn Pathol. 2021;54. doi:https://doi.org/10.1016/j.anndiagpath.2021.151787
- De Luca P, Di Stadio A, Petruzzi G. A multicenter protocol to assess the prognostic significance of the tumor microenvironment in patients with squamous cell carcinoma of the larynx. Head Neck. 2024;46:2123-2131. doi:https://doi.org/10.1002/hed.27860
- Chatzopoulos K, Kotoula V, Manoussou K. Tumor infiltrating lymphocytes and CD8+ T cell subsets as prognostic markers in patients with surgically treated laryngeal squamous cell carcinoma. Head Neck Pathol. 2020;14:689-700. doi:https://doi.org/10.1007/s12105-019-01101-6
- Lewis J, Ukpo O, Ma X-J. Transcriptionally-active high-risk human papillomavirus is rare in oral cavity and laryngeal/hypopharyngeal squamous cell carcinomas – A tissue microarray study utilizing E6/E7 mRNA in situ hybridization. Histopathology. 2012;60:982-991. doi:https://doi.org/10.1111/j.1365-2559.2011.04169-x
- De Luca P, de Campora L, Gallo O. “Almost Forty!”: four decades of open partial horizontal laryngectomy – The evolving experience of the Italian school of Enrico de Campora. Head Neck. 2025;47:1364-1371. doi:https://doi.org/10.1002/hed.28041
- Govender R, Lee M, Davies T. Development and preliminary validation of a patient-reported outcome measure for swallowing after total laryngectomy (SOAL questionnaire). Clin Otolaryngol. 2012;37:452-459. doi:https://doi.org/10.1111/coa.12036
- Govender R, Lee M, Drinnan M. Psychometric evaluation of the Swallowing Outcomes After Laryngectomy (SOAL) patient-reported outcome measure. Head Neck. 2016;38:E1639-E1645. doi:https://doi.org/10.1002/hed.24291
- Beaton D, Bombardier C, Guillemin F. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25:3186-3191. doi:https://doi.org/10.1097/00007632-200012150-00014
- Taft T, Riehl M, Sodikoff J. Development and validation of the brief esophageal dysphagia questionnaire. Neurogastroenterol Motil. 2016;28:1854-1860. doi:https://doi.org/10.1111/nmo.12889
- Chen A, Frankowski R, Bishop-Leone J. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M.D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. 2001;127:870-876.
- Cichero J. Age-related changes to eating and swallowing impact frailty: aspiration, choking risk, modified food texture and autonomy of choice. Geriatrics (Basel). 2018;3. doi:https://doi.org/10.3390/geriatrics3040069
- Serra-Prat M, Hinojosa G, López D. Prevalence of oropharyngeal dysphagia and impaired safety and efficacy of swallow in independently living older persons. J Am Geriatr Soc. 2011;59:186-187. doi:https://doi.org/10.1111/j.1532-5415.2010.03227.x
- Mathlin J, Courtier N, Hopkinson J. Taste changes during radiotherapy for head and neck cancer. Radiography (Lond). 2023;29:746-751. doi:https://doi.org/10.1016/j.radi.2023.05.004
- Ma Y, Green R, Pan S. Long-term voice outcome following radiation versus laser microsurgery in early glottic cancer. J Voice. 2019;33:176-182. doi:https://doi.org/10.1016/j.jvoice.2017.10.018
- Yılmaz T. Voice after cordectomy Type I or Type II or radiation therapy for large T1a glottic cancer. Otolaryngol Head Neck Surg. 2023;168:798-804. doi:https://doi.org/10.1177/01945998221117453
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 543 times
- PDF downloaded - 132 times



