Reviews
Vol. 45: Issue 5 - October 2025
A systematic review and network meta-analysis of therapies for locally advanced head and neck squamous cell carcinoma with different HPV status
Abstract
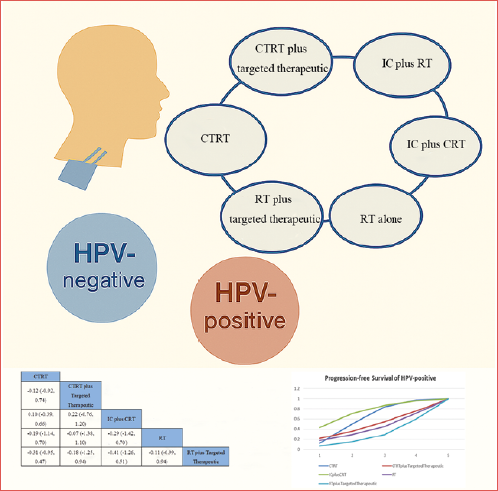
Infection with high-risk human papillomavirus (HPV) is considered a major cause of head and neck squamous cell carcinoma (HNSCC). However, the optimal treatment choice remains uncertain for both HPV-positive and HPV-negative locally advanced HNSCC (LA-HNSCC) in patients who are unable to tolerate surgery. To assess the effectiveness of various treatment strategies for HPV-positive and HPV-negative LA-HNSCC, this systematic review and network meta-analysis evaluated 4 databases and identified 31 relevant studies. The selected outcomes included overall survival, progression-free survival, locoregional control, distant metastasis, and disease-free survival. Hazard ratios with 95% confidence intervals were pooled for each outcome, and treatment modality rankings were calculated using the surface under the cumulative ranking curve. We found that induction chemotherapy combined with radiotherapy and chemoradiotherapy were optimal for HPV-positive patients, while concurrent chemoradiotherapy and concurrent chemoradiotherapy combined with targeted therapy were most effective for HPV-negative patients. These findings highlight the importance of individualised treatment protocols and lay the groundwork for future clinical trials to optimise outcomes in LA-HNSCC.
Introduction
Head and neck squamous cell carcinomas (HNSCC) represents a major global health burden due to its high rates of morbidity and mortality, and is the sixth most common cancer worldwide 1, with the majority of cases being diagnosed at a locally advanced stage. Locally advanced HNSCC (LA-HNSCC) is defined by categories T3/4 and N1-3, with a clinical stage of III/IV 2,3. LA-HNSCC is associated with poor prognosis, high recurrence rates, and low 5-year survival. Functional outcomes, such as speech and swallowing abilities, are often significantly impaired following long-term treatment, frequently necessitating multidisciplinary care 4-6. Treatment for LA-HNSCC typically includes chemotherapy, surgery, and systemic therapy. However, certain cases of LA-HNSCC are unsuitable for surgical intervention due to the tumour’s location, extent, or associated comorbidities. Compared with radiotherapy (RT) alone, concurrent chemoradiotherapy (CTRT) significantly improves survival rates and quality of life for patients with LA-HNSCC, and is generally considered as standard treatment 7-9. However, chemotherapy, particularly platinum-based agents, often causes severe adverse events in the early stages of treatment 10,11. Consequently, induction chemotherapy (IC) has been proposed for patients with LA-HNSCC although its benefits remain controversial 12,13. Additionally, the epidermal growth factor receptor (EGFR) had been identified as a therapeutic target for HNSCC, and targeted therapies had been used in patients with LA-HNSCC, showing associations with improved prognosis 14,15. Despite these promising findings, randomised trials indicate that cetuximab does not significantly improve overall survival (OS) in patients with LA-HNSCC. Importantly, the addition of cetuximab has been associated with poorer prognostic outcomes 16. Currently, advances in understanding the tumour immune microenvironment have propelled immunotherapy to the forefront of research. Immunotherapy has achieved certain advancements in the treatment of recurrent or metastatic HNSCC 17. However, it has not yet been incorporated as a first-line treatment for LA-HNSCC. Although current multimodal treatments have provided more therapeutic options for LA-HNSCC, concerns persist regarding the increased toxicity associated with these regimens. The optimal treatment approach for LA-HNSCC remains controversial.
Traditionally, tobacco and alcohol use have been regarded as key risk factors in the development and progression of HNSCC 18. However, recent studies indicate that the incidence of HNSCC without abuse of tobacco and alcohol has been increasing over the years 19,20. Infection with high-risk human papillomavirus (HPV) has become a major cause of HNSCC, alongside smoking and alcohol consumption 21. Notably, HPV is predominantly associated with a subset of oropharyngeal squamous cell carcinoma (OPSCC). Globally, approximately 33% of OPSCC cases are HPV-positive 22. Importantly, HPV-positive and HPV-negative HNSCC differ in clinical presentation, prognosis, and response to treatment 23,24. HPV-positive HNSCC primarily occurrs in the oropharynx and is characterised by lower recurrence rates and better prognosis, prompting active exploration of treatment strategies for HPV-positive HNSCC 22,25. In contrast, HPV-negative HNSCC is linked to traditional risk factors, such as tobacco and alcohol use, and typically follows a more aggressive course with poorer outcomes 4,25. Globally, especially in developing countries, HPV-negative HNSCC remains the predominant form, driving continuous efforts to develop more aggressive combination therapies 26,27.
Despite advances in multimodal therapy, including surgery, RT, chemotherapy, and targeted agents, the optimal treatment approach for both HPV-positive and HPV-negative LA-HNSCC remains controversial. The lack of a standardised regimen tailored to the biological differences of these two subtypes poses significant clinical challenges 28,29. Given these complexities, understanding how each therapeutic strategy performs in HPV-positive and HPV-negative LA-HNSCC is critical for advancing personalised treatments.
This systematic review and network meta-analysis aims to fill this gap by evaluating the following six treatment strategies: IC followed by RT, RT combined with targeted therapy, IC followed by chemoradiotherapy, CTRT, CTRT combined with targeted therapy, and RT alone. By comparing the relative efficacy of different treatment strategies for HPV-positive and HPV-negative LA-HNSCC, this analysis provides evidence-based insights to guide clinical decision-making.
Materials and methods
This systematic review has been prospectively registered in the International Prospective Register of Systematic Reviews (registration number: CRD42024590601) and was carried out in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement 30.
Search strategy
We conducted the systematic review using four electronic databases: PubMed, EMBASE, Web of Science, and the Cochrane Library. The results were reported following the PRISMA guidelines, with the final search completed on July 20, 2024. The search employed key terms such as “head and neck squamous cell carcinoma,” and “human papillomavirus.” The complete search strategy is provided in the supplementary section (Tab. SI). There were no restrictions on language or publication type, and only full-text articles were considered. Additionally, we manually reviewed the reference lists of primary studies and review papers to identify other relevant studies.
Inclusion and exclusion criteria
The inclusion criteria for this meta-analysis were: (1) studies comparing different treatment strategies for HPV-positive and HPV-negative LA-HNSCC in pairwise comparisons; (2) phase II/III randomised controlled trials (RCTs); (3) patients diagnosed with LA-HNSCC (Stage III/IV); (4) no surgical treatment options; (5) HPV status determined through immunohistochemical detection of p16, in situ hybridisation, or real-time quantitative PCR targeting HPV nucleic acids.
Exclusion criteria were: (1) duplicate publications, abstract-only papers, editorial commentaries, letters, case reports, reviews, meta-analyses, and irrelevant titles or abstracts; (2) studies with incomplete or unclear data; (3) when patient populations overlapped between studies, only the most recent publication was included.
Quality assessment
We assessed the risk of bias using the Cochrane Collaboration’s tool 31, covering domains such as random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential biases. Each study was classified as having a high, low, or unclear risk of bias. Two authors independently evaluated each domain, with a third author resolving any disagreements.
Data extraction
All data were independently collected by two reviewers. The following study characteristics were recorded for each trial: (1) study and patient characteristics, including staging, histology, and methods of HPV group classification; (2) number of patients per group and treatment regimens; and (3) reported outcome measures, including OS, progression-free survival (PFS), locoregional control (LRC), distant metastasis (DM), and disease-free survival (DFS).
Statistical analysis
The primary endpoint of our network meta-analysis was OS, with additional endpoints including PFS, LRC, DM, and DFS. For survival analysis, the preferred outcome measure was the unadjusted hazard ratio (HR) with the corresponding 95% confidence interval (CI). HR and 95% CI were extracted and transformed into log HR and corresponding standard error to obtain the Summary HR (SHR). When necessary HR were also derived from published survival curves by accurately extracting curve coordinates using digitisation software (DigitizeIt) 32. These coordinates were then used to generate summary statistics according to Parmar’s method 33. Furthermore, the rankings of different treatment strategies were calculated by the surface under the cumulative ranking curve (SUCRA), which ranges from 0 to 1, with higher values indicating more favourable treatment outcomes.
The I² statistic was used to assess heterogeneity across studies, with values above 50% indicating high heterogeneity. Random effects were employed, using an identity link function and non-informative priors (uniform and normal distributions) to fit the model. Posterior distributions of the model parameters were obtained through 25,000 iterations, with a burn-in of 5,000 iterations and a thinning interval of 20. Convergence was assessed using the Brooks-Gelman-Rubin method. Posterior distributions were used to estimate the probabilities of each treatment being the best, second-best, and so on. Effect sizes in the Bayesian network meta-analysis were described using 95% credible regions (CR). The probability of each strategy being the best was calculated by ranking the relative efficacy of all interventions across iterations and determining the proportion of iterations in which each strategy ranked first. All analyses were conducted using the R packages “Metaphor” and “Gemtc” (https://www.r-project.org/). In addition, this study employed a meta-regression approach, using the proportion of smokers as the independent variable and the log-transformed HR (log HR) as the dependent variable. Separate meta-regression models were fitted for two clinical endpoints: OS and PFS. A random-effects linear meta-regression model was used to evaluate the association between the proportion of smokers and survival outcomes by estimating the regression coefficients, standard errors, t values, p values, and 95% CI.
Results
Study selection
We searched four databases, retrieving a total of 21,903 initial records. After removing duplicates, 14,320 records remained. After screening titles and abstracts, 142 articles were identified for further evaluation. Following detailed assessment, 111 articles were excluded: 36 lacked extractable survival data, 29 involved non-locally advanced cancer, 35 did not perform HPV subgroup comparisons, 5 were systematic reviews, meta-analyses, commentaries, or letters, 2 were duplicates, and 4 had unavailable full texts. Ultimately, 31 studies were included 34-64. Figure 1 presents the PRISMA flow diagram illustrating the study selection process.
Summary of included studies and quality assessment
A total of 31 studies were included, comprising 5779 cases with HPV-positive and 2921 cases with HPV-negative cancer. HPV diagnostic tests included immunohistochemical p16, PCR, and in situ hybridisation for detecting HPV nucleic acids. Three studies did not specify the methods used for HPV differentiation. Of the 31 studies, 3 involved three comparison groups, while the rest compared two groups. The interventions included CTRT, CTRT plus targeted therapy, RT alone, RT plus targeted therapy, IC plus CRT and IC plus RT. Table I outlines the study details and the interventions used for both control and experimental groups.
The overall quality of the included trials ranged from moderate to high, as depicted in Supplementary Figure 1 and Supplementary Figure 2, we identified a high risk of performance bias in 10 RCTs, while the remaining RCTs exhibited a low risk of bias. Most studies did not explicitly indicate whether allocation concealment was implemented, and some studies did not provide sufficient information to assess the presence of random sequence generation and selective reporting biases. In addition, smoking status data specific to HPV-positive patients were extracted, with 12 studies reporting smoking behaviour among individuals with HPV-positive HNSCC (Tab. II).
Outcomes
OVERALL SURVIVAL
A total of 21 studies were included in this research, with 19 reporting HPV-positive HNSCC. Among these, two studies involved comparisons between three intervention groups, with a combined sample size of 4137 cases and overall heterogeneity was I² = 18% (Fig. 2A). Ten studies reported on HPV-negative cases, including one study comparing three intervention groups, with a total sample size of 1000 cases, and the overall heterogeneity was I² = 15% (Fig. 2B). In HPV-positive HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3A, 4A). The ranking based on Surface Under the Cumulative Ranking curve (SUCRA) was as follows: IC plus RT (SUCRA = 83.3%) was the most effective in improving OS among HPV-positive patients, followed by RT plus Targeted Therapeutic (SUCRA = 78.7%), CTRT (SUCRA = 58.9%), IC plus CRT (SUCRA = 58%), RT alone (SUCRA = 42.6%), and CTRT plus Targeted Therapeutic (SUCRA = 30.3%) (Fig. 5A).
In HPV-negative HNSCC, as shown in the forest plots and league tables, the results did not indicate statistically significant differences (Figs. 3B, 4B). According to the ranking plot (Fig. 5B), among HPV-negative patients, CTRT (SUCRA = 82.7%) was the most effective, followed by CTRT plus Targeted Therapeutic (SUCRA = 71.9%), IC plus CRT (SUCRA = 58.1%), RT plus Targeted Therapeutic (SUCRA = 44.1%), and RT alone (SUCRA = 43%).
PROGRESSION-FREE SURVIVAL
A total of 14 studies were included in the analysis, with 12 reporting on HPV-positive HNSCC, involving a total of 2183 cases. The overall heterogeneity was I² = 20% (Fig. 2C). Seven studies reported on HPV-negative cases, with a total of 1229 cases. The overall heterogeneity was I² = 21% (Fig. 2D). In HPV-positive HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3C, 4C). According to the ranking plot (Fig. 5C), for HPV-positive HNSCC, IC plus CRT (SUCRA = 81.2%) and CTRT (SUCRA = 71.8%) were the most effective treatments, followed by CTRT plus Targeted Therapeutic (SUCRA = 56.7%), RT alone (SUCRA = 51.2%), and RT plus Targeted Therapeutic (SUCRA = 39.1%).
In HPV-negative HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3D, 4D). According to the ranking plot (Fig. 5D), for HPV-negative HNSCC, the treatments were ranked as follows: CTRT (SUCRA = 84.4%), CTRT plus Targeted Therapeutic (SUCRA = 70.9%), and IC plus CRT (SUCRA = 44.5%).
LOCO-REGIONAL CONTROL
A total of 5 studies were included, all of which reported on HPV-positive HNSCC with a total of 506 cases. The overall heterogeneity was I² = 26% (Fig. 2E). Five studies reported on HPV-negative cases, with a total of 497 cases. The overall heterogeneity was I² = 0% (Fig. 2F). In HPV-positive HNSCC, as shown in the forest plots and league tables, the results did not indicate statistically significant differences (Fig. 3E, 4E). According to the ranking plot for HPV-positive HNSCC (Fig. 5E), the treatments were ranked as follows: CTRT (SUCRA = 91.3%) was the most effective, followed by RT plus Targeted Therapeutic (SUCRA = 73.4%) and RT alone (SUCRA = 35.1%).
In HPV-negative HNSCC, as shown in the forest plots and league tables, the results did not indicate statistically significant differences (Figs. 3F, 4F). According to the ranking plot for HPV-negative HNSCC (Fig. 5F), the order is as follows: RT plus Targeted Therapeutic (SUCRA = 85.9%), CTRT (SUCRA = 85%), RT alone (SUCRA = 51.7%) and CTRT plus Targeted Therapeutic (SUCRA = 27.3%).
DISTANT METASTASES
A total of 7 studies were included in this research, with 4 reporting on HPV-positive HNSCC, involving a total of 1841 cases. The overall heterogeneity was I² = 30% (Fig. 2G). Three studies reported on HPV-negative cases, including one study comparing three intervention groups, with a total sample size of 616 cases and an overall heterogeneity of I² = 16% (Fig. 2H). In HPV-positive HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3G, 4G). According to the ranking plot for HPV-positive HNSCC: IC plus CRT (SUCRA = 90.4%), RT alone (SUCRA = 78.2%), CTRT (SUCRA = 56.9%) and RT plus Targeted Therapeutic (SUCRA = 24.4%) (Fig. 5G).
In HPV-related HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3H, 4H). According to the ranking plot for HPV-negative cases (Fig. 5H), CTRT plus targeted therapy (SUCRA = 84.3%) ranks highest, followed by RT plus targeted therapy (SUCRA = 77.2%), RT alone (SUCRA = 53.7%), and CTRT (SUCRA = 34.7%).
DISEASE-FREE SURVIVAL
A total of 6 studies were included in the research, with four reporting HPV-positive HNSCC, comprising 397 cases in total. The overall heterogeneity was I² = 35% (Fig. 2I). Three studies focused on HPV-negative cases, with a total of 410 cases and an overall heterogeneity of I² = 28% (Fig. 2J). In HPV-positive HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3I, 4I). For HPV-positive HNSCC, the ranking based on SUCRA was as follows (Fig. 5I): RT alone (SUCRA = 65.5%) and CTRT (SUCRA = 65.5%) were the most effective treatments, followed by RT plus targeted therapy (SUCRA = 62.4%) and CTRT plus targeted therapy (SUCRA = 56.5%).
In HPV-negative HNSCC, according to the forest plots and the league table, the results were not statistically significant (Figs. 3J, 4J). According to the ranking chart for HPV-negative HNSCC (Fig. 5J), the treatment hierarchy was as follows: CTRT plus targeted therapy (SUCRA = 85.7%), IC plus CRT (SUCRA = 81.7%) and CTRT (SUCRA = 32.4%).
The meta-regression analysis yielded positive coefficients for both PFS and OS (0.34 and 0.45, respectively), indicating a possible association between higher smoking prevalence and increased hazard (Fig. 6). However, in the meta-regression analysis, both PFS and OS were associated with large standard errors and wide 95% CIs (PFS: −5.09 to 5.78; OS: −7.72 to 8.61), resulting in no statistically significant associations (p > 0.05) (Tab. III).
Discussion
Currently, LA-HNSCC continues to show high recurrence and metastasis rates, with poor prognosis, leading to ongoing debate regarding the optimal treatment strategy 6. As a primary aetiological factor, HPV infection is correlated with prognosis of HNSCC 23,24. HPV is predominantly associated with a subset of OPSCC. To date, no treatment regimen has been tailored to address the biological differences between HPV-positive and HPV-negative LA-HNSCC. This study systematically compared the outcomes of various therapeutic strategies for HPV-positive and HPV-negative LA-HNSCC across 5 key endpoints: OS, PFS, LRC, DM and DFS. These outcomes underscore the clinical importance of tailoring treatment strategies based on HPV status, as different patterns emerged between the two subtypes.
For OS, IC plus RT was the most effective therapeutic approach for HPV-positive HNSCC, while CTRT proved to be the best for HPV-negative HNSCC. For PFS, HPV-positive HNSCC demonstrated longer PFS compared to HPV-negative patients, with IC plus CRT being the most effective for HPV-positive HNSCC and CTRT leading to the best results for HPV-negative HNSCC. In terms of LRC, HPV-positive HNSCC also fared better in loco-regional control, particularly with CTRT, which was the most effective in controlling local tumour growth. Conversely, in HPV-negative HNSCC, RT plus targeted therapies provided better loco-regional control, reflecting the need to address the more aggressive and widespread nature of HPV-negative HNSCC. In terms of DM, the patterns further differentiate the two subtypes. HPV-positive HNSCC experienced lower rates of distant metastasis, with IC plus CRT being the most effective in reducing DM. In contrast, HPV-negative HNSCC exhibited higher rates of distant metastasis, necessitating the use of CTRT plus targeted therapy to achieve better control. DFS outcomes also varied between HPV-positive and HPV-negative HNSCC. For HPV-positive HNSCC, RT alone or CTRT provided the most effective control, resulting in longer DFS. For HPV-negative HNSCC, CTRT plus targeted therapy was the most effective in improving DFS.
CTRT is considered the standard treatment regimen for LA-HNSCC 7, combining chemotherapy with radiotherapy to improve clinical prognosis. According to this study, CTRT showed the highest effectiveness in HPV-negative HNSCC compared with other treatment approaches. The addition of targeted therapy did not improve OS or PFS for HPV-negative LA-HNSCC, which may be attributed to the relative rarity of EGFR pathway alterations in HPV-negative LA-HNSCC 66-69. However, given the more aggressive nature and broader spread of HPV-negative HNSCC, adding targeted therapy could potentially achieve better LRC and reduce DM, leading to improved survival and progression control. For HPV-positive LA-HNSCC, IC plus RT was more effective in improving OS than other treatment strategies. This enhanced outcome may be stemmed from HPV infection’s impact on cell cycle and apoptosis pathways, as well as its effect on DNA damage response and repair mechanisms, which increases the tumour’s responsiveness to DNA-damaging treatments like radiotherapy 70,71. The addition of IC prior to RT or CTRT improved OS and PFS in HPV-positive HNSCC. IC enhanced the efficacy of subsequent RT and CTRT 12, the systemic control achieved through induction chemotherapy, followed by aggressive radiotherapy, played a critical role in reducing DM in HPV-negative HNSCC. HPV-positive LA-HNSCC, driven by viral oncogenesis, exhibits heightened radiosensitivity and immunogenicity, making these tumours more responsive to radiotherapy 70-72. Consequently, unlike HPV-negative HNSCC, adding targeted therapy failed to significantly improve LRC, reduce DM, or maintain DFS in HPV-positive LA-HNSCC.
Elhalawani et al. identified that OS in HPV-positive HNSCC patients is significantly affected by tobacco exposure, particularly in those with a smoking history of more than 30 pack-years 73. However, among the studies included in this research, only 12 stratified HPV-positive patients by smoking status, and none conducted subgroup analyses specifically for HPV-positive smokers. Thus, the meta-regression was performed to assess the association between smoking prevalence and survival outcomes. Although the regression coefficients for PFS and OS were both positive (0.34 and 0.45, respectively), this analysis did not identify a statistically significant relationship between smoking prevalence and survival outcomes in HPV-positive HNSCC. The lack of statistical significance is likely due to the limited number of studies included in the regression analysis. Future studies that include high-quality research clearly reporting smoking stratification could help to further validate these findings.
Compared with previous meta-analyses, which often grouped all HNSCC cases together, this study’s strengths lay in its stratification by HPV status, providing more specific insights into treatment efficacy. Earlier meta-analyses failed to account for the distinct biology of HPV-positive and HPV-negative disease, potentially leading to less informative treatment recommendations. Our use of a network meta-analysis framework also allowed for comprehensive comparisons across multiple therapeutic options, including indirect comparisons where direct head-to-head trials were unavailable. This approach enhanced the robustness of our findings and provides more nuanced guidance for clinical decision-making. Additionally, the inclusion of a broad range of outcomes, such as loco-regional control and distant metastases, offers a more complete picture of therapeutic efficacy.
Despite the strengths of this analysis, several limitations must be considered. First, although we conducted risk-of-bias assessments and included only moderate to high-quality studies, the potential for bias cannot be entirely excluded. The included studies differ in terms of patient follow-up duration, treatment methods, and other factors, which may affect the integration of results, especially regarding variations in HPV testing methods. Additionally, the lack of individual patient data was a limitation. Since this study is based on aggregated data rather than individual-level data, we failed to explore the potential relationships between patient characteristics (e.g., primary tumour site, age, gender, HPV viral load) and treatment outcomes in detail. Specifically, although HPV infection has been detected in hypopharyngeal, oral, and laryngeal squamous cell carcinoma, it is primarily associated with a subset of OPSCC 22,74. Due to the inability of the included studies to accurately report sub-site data, subgroup analysis could not be performed. For instance, the studies by Harrington et al. and Mesía et al. did not specify the pathological subtypes of HPV-positive HNSCC 34,35. Therefore, in future research, we will conduct further investigations by stratifying based on tumour site to explore the impact of this factor on the outcomes more effectively. Furthermore, although this study acknowledges the increasing role of immunotherapy in the management of recurrent or metastatic HNSCC, the exclusion of immunotherapy from our analysis represents a significant limitation. Consequently, future studies should investigate how immunotherapy could be effectively integrated with traditional treatments, such as CTRT. This combined approach holds promise for improving patient outcomes in HNSCC treatment.
Conclusions
In summary, this systematic review and network meta-analysis highlighted the importance of tailoring treatment strategies to the HPV status of HNSCC patients. IC plus RT and IC plus CRT emerged as leading strategies for HPV-positive patients, while CTRT and CTRT plus targeted therapeutic were most effective for HPV-negative cases. These findings underscore the need for personalised treatment protocols that account for the distinct biology of these subtypes. However, further research is required to refine these strategies, particularly in light of emerging therapies and the need to balance efficacy with toxicity.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This work was supported by The National Natural Science Foundation of China (NSFC, 82360499), and the science and the technology department of Guizhou Province, Basic Research Program (Natural Science Category) (Qiankehe Foundation -ZK[2023] General 574).
Author contributions
MC: data curation, formal analysis, methodology, software, writing – original draft; CZ: data curation, software, writing – original draft. CR: formal analysis, methodology, writing – original draft; CL: conceptualization, supervision, validation, visualization, writing – review & editing. All authors contributed to the manuscript and approved the final version for submission.
Ethical consideration
Not applicable.
History
Received: April 3, 2025
Accepted: June 30, 2025
Figures and tables
Figure 1. PRISMA flow diagram illustrating the study selection process.
Figure 2. Network diagrams: (A) comparing overall survival of HPV-positive HNSCC patients with different treatment options; (B) network diagram comparing overall survival of HPV-negative HNSCC patients; (C) progression-free survival of HPV-positive HNSCC patients; (D) progression-free survival of HPV-negative HNSCC patients; (E) loco-regional control of HPV-positive HNSCC patients; (F) loco-regional control of HPV-negative HNSCC patients; (G) distant metastases of HPV-positive HNSCC patients; (H) distant metastases of HPV-negative HNSCC patients; (I) disease-free survival of HPV-positive HNSCC patients; (J) disease-free survival of HPV-negative HNSCC patients.
Figure 3. Forest plots: (A) showing overall survival for different treatments in HPV-positive head and neck squamous cell carcinoma (hazard ratios and 95% CI); (B) overall survival for different treatments in HPV-negative head and neck squamous cell carcinoma (hazard ratios and 95% CI); (C) progression-free survival for different treatments in HPV-positive head and neck squamous cell carcinoma (hazard ratios and 95% CI); (D) progression-free survival for different treatments in HPV-negative head and neck squamous cell carcinoma (hazard ratios and 95% CI); (E) loco-regional control for different treatments in HPV-positive head and neck squamous cell carcinoma (hazard ratios and 95%CI); (F) loco-regional control for different treatments in HPV-negative head and neck squamous cell carcinoma (hazard ratios and 95% CI); (G) distant metastases for different treatments in HPV-positive head and neck squamous cell carcinoma (hazard ratios and 95% CI); (H) distant metastases for different treatments in HPV-negative head and neck squamous cell carcinoma (hazard ratios and 95%CI); (I) disease-free survival for different treatments in HPV-positive head and neck squamous cell carcinoma (hazard ratios and 95% CI); (J) disease-free survival for different treatments in HPV-negative head and neck squamous cell carcinoma (hazard ratios and 95% CI).
Figure 4. The league table: (A) showing overall survival for different treatments in HPV-positive head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (B) overall survival for different treatments in HPV-negative head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (C) progression-free survival for different treatments in HPV-positive head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (D) progression-free survival for different treatments in HPV-negative head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (E) loco-regional control for different treatments in HPV-positive head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (F) loco-regional control for different treatments in HPV-negative head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (G) distant metastases for different treatments in HPV-positive head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (H) distant metastases for different treatments in HPV-negative head and neck squamous cell carcinoma (summary hazard ratios and 95% CI); (I) the league table showing disease-free survival for different treatments in HPV-positive head and neck squamous cell carcinoma(summary hazard ratios and 95% CI); (J) disease-free survival for different treatments in HPV-negative head and neck squamous cell carcinoma (summary hazard ratios and 95% CI).
Figure 5. The rank plot: (A) showing overall survival for different treatments in HPV-positive head and neck squamous cell carcinoma; (B) overall survival for different treatments in HPV-negative head and neck squamous cell carcinoma; (C) progression-free survival for different treatments in HPV-positive head and neck squamous cell carcinoma; (D) progression-free survival for different treatments in HPV-negative head and neck squamous cell carcinoma; (E) loco-regional control for different treatments in HPV-positive head and neck squamous cell carcinoma; (F) loco-regional control for different treatments in HPV-negative head and neck squamous cell carcinoma; (G) distant metastases for different treatments in HPV-positive head and neck squamous cell carcinoma; (H) distant metastases for different treatments in HPV-negative head and neck squamous cell carcinoma; (I) disease-free survival for different treatments in HPV-positive head and neck squamous cell carcinoma; (J) disease-free survival for different treatments in HPV-negative head and neck squamous cell carcinoma.
Figure 6. Meta-regression analysis of the association between smoking prevalence and survival outcomes in HPV-positive patients: (A) overall survival for HPV-positive HNSCC; (B) progression-free survival for HPV-positive HNSCC.
Figure S1. Risk of bias graph.
Figure S2. Risk of bias summary.
| Author | Year | Experimental arm | Control arm | Control arm | Cancer site | Stage | Determination of HPV status | HPV-positive | HPV-negative | Evaluated endpoints | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Harrington 34 | 2012 | CTRT plus targeted therapeutic | CTRT | / | Oral cav | III/IVA | IHC-p16 | 7 | 30 | PFS | / | / | |
| Mesía 35 | 2015 | CTRT | CTRT plus targeted therapeutic | / | Oral cav | III/IVA | IHC-p16 | 42 | 57 | PFS | OS | / | |
| Strom 36 | 2015 | CTRT | RT plus targeted therapeutic | / | Oral cav | III/IVA | IHC-p16 | 99 | 49 | LRC | OS | / | |
| Tang 37 | 2015 | RT plus targeted therapeutic | CTRT plus targeted therapeutic | CTRT | Oral cav | III/IV | IHC-p16 | 103 | 74 | OS | / | / | |
| Nien 38 | 2016 | CTRT | RT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 339 | 0 | OS | / | / | |
| Ou 39 | 2016 | CTRT | RT plus targeted therapeutic | / | Oral cav | III/IV (97%) | IHC-p16 | 88 | 177 | PFS | LRC | / | |
| Rosenthal 30 | 2016 | RT | RT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 107 | 63 | PFS | OS | LRC | |
| Adkins 41 | 2017 | CTRT plus targeted therapeutic | CTRT | / | Oropharynx | III/IV | IHC-p16 | 34 | 26 | OS | / | / | |
| Buglione 42 | 2016 | CTRT | RT plus targeted therapeutic | / | Oropharynx | III/IVA | IHC-p16 | 7 | 21 | / | LRC | OS | |
| Barney 43 | 2018 | CTRT | RT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 205 | 0 | OS | LRC | DFS | |
| Onita 44 | 2018 | RT plus targeted therapeutic | CTRT | / | Oropharynx | III | IHC-p16 | 291 | 0 | DM | / | / | |
| Gillison 45 | 2019 | RT plus targeted therapeutic | CTRT | / | Oropharynx | III/IV | IHC-p16 | 805 | 0 | OS | PFS | DM | |
| Mehanna 46 | 2019 | CTRT | RT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 334 | 0 | OS | / | / | |
| Patil 47 | 2019 | CTRT | CTRT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 24 | 187 | / | PFS OS LRC DFS | ||
| Beckham 48 | 2020 | CTRT | RT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 0 | 316 | OS | DM | / | |
| Jeong 49 | 2020 | CTRT | RT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 55 | 16 | OS | / | / | |
| Lee 50 | 2021 | CTRT plus targeted therapeutic | CTRT | / | Oropharynx | III/IV | IHC-p16 | 338 | 459 | PFS | / | / | |
| Rischin 51 | 2021 | RT plus targeted therapeutic | CTRT | / | Oropharynx | III/IV | IHC-p16 | 182 | 0 | OS | / | / | |
| Yom 52 | 2021 | RT | CTRT | / | Oropharynx | III/IV | IHC-p16 | 306 | 0 | PFS | OS | DM | |
| Wong 53 | 2023 | CTRT | CTRT plus targeted therapeutic | / | Oropharynx | III/IV | IHC-p16 | 0 | 127 | OS | PFS | DM | |
| Sher 54 | 2016 | CTRT | IC plus RT | / | Oropharynx | III/IV | PCR | 984 | 815 | OS | / | / | |
| Bhattasali 55 | 2018 | IC plus RT | CTRT | / | Oropharynx | III/IV | IHC-p16 | 87 | 0 | OS | PFS | DM | |
| Lorch 56 | 2016 | CTRT | IC plus RT | / | Oropharynx | III/IV | IHC-p16 PCR | 164 | 138 | OS | PFS | / | |
| Dobrosotskaya 57 | 2013 | IC plus RT | CTRT | / | Oropharynx | III/IV | PCR | 54 | 16 | OS | / | / | |
| Mercke 58 | 2023 | IC plus RT | CTRT | / | Oropharynx tonsil base of tongue | III/IV | IHC-p16 PCR | 150 | 0 | OS | PFS | / | |
| Geoffrois 59 | 2018 | IC plus RT | CTRT | / | Oropharynx | III/IV | IHC-p16 | 45 | 127 | PFS | / | / | |
| Golubev 60 | 2023 | IC plus RT | CTRT | / | Oropharynx | III/IV | IHC-p16 | 27 | 0 | PFS | / | / | |
| Hall 61 | 2018 | CTRT | RT | / | Oropharynx | III/IV (82%) | IHC-p16 ISH | 352 | 173 | DM | / | / | |
| Burtness 62 | 2019 | CTRT plus targeted therapeutic | CTRT | / | Oropharynx hypopharynx larynx oral cavity | III/IV | IHC-p16 | 94 | 196 | DFS | / | / | |
| De Felice 63 | 2016 | IC plus RT | CTRT | / | Oropharynx | III/IV | / | 0 | 27 | DFS | / | / | |
| Riaz 64 | 2016 | RT plus targeted therapeutic | CTRT | / | Oropharynx | III/IV | IHC-p16 | 182 | 0 | OS | / | / | |
| RT radiotherapy; CTRT: concurrent chemoradiation therapy; IC plus CRT: induction chemotherapy plus chemoradiotherapy; IHC-p16: | |||||||||||||
| p16 immunohistochemistry; ISH: in situ hybridisation; PCR: polymerase chain reaction; OS: overall survival; PFS: progression-free survival; | |||||||||||||
| LRC: locoregional control; DM: distant metastasis; DFS: disease-free survival. | |||||||||||||
| Author | Year | Experimental arm | Control arm | Control arm | HPV-positive | ||
|---|---|---|---|---|---|---|---|
| Smoker | Nonsmoker | Evaluated endpoints | |||||
| Tang 37 | 2015 | RT plus targeted therapeutic | CTRT plus targeted therapeutic | CTRT | 103 | 74 | / |
| Nien 38 | 2016 | CTRT | RT plus targeted therapeutic | / | 177 | 162 | / |
| Barney 43 | 2018 | CTRT | RT plus targeted therapeutic | / | 205 | 0 | DFS |
| Gillison 45 | 2019 | RT plus targeted therapeutic | CTRT | / | 430 | 375 | DM |
| Mehanna 46 | 2019 | CTRT | RT plus targeted therapeutic | / | 154 | 180 | / |
| Rischin 51 | 2021 | RT plus targeted therapeutic | CTRT | / | 71 | 111 | / |
| Yom 52 | 2021 | RT | CTRT | / | 93 | 213 | DM |
| Bhattasali 55 | 2018 | IC plus CRT | CTRT | / | 18 | 69 | DM |
| Mercke 58 | 2023 | IC plus CRT | CTRT | / | 53 | 97 | / |
| Geoffrois 59 | 2018 | IC plus CRT | CTRT | / | 37 | 8 | / |
| Ou 39 | 2016 | CTRT | RT plus targeted therapeutic | / | 63 | 25 | / |
| Golubev 60 | 2023 | IC plus CRT | CTRT | / | 12 | 15 | / |
| RT: radiotherapy; CTRT: concurrent chemoradiation therapy; IC plus CRT: induction chemotherapy plus chemoradiotherapy; DM: distant metastasis; DFS: disease-free survival. | |||||||
| Outcomes | Variable | Coefficient | Standard error | t | p > |t| | 95% confidence interval lower | 95% confidence interval upper |
|---|---|---|---|---|---|---|---|
| PFS | smoking | 0.34 | 1.26 | 0.27 | 0.81 | -5.09 | 5.78 |
| OS | smoking | 0.45 | 2.94 | 0.15 | 0.89 | -7.72 | 8.61 |
| Search strategy | |||
|---|---|---|---|
| Pubmed | 1 | (“Squamous Cell Carcinoma of Head and Neck”[Mesh]) | 12146 |
| 2 | (“Squamous Cell Carcinoma of Head and Neck” OR “Head And Neck Squamous Cell Carcinomas” OR “Squamous Cell Carcinoma, Head And Neck” OR “Squamous Cell Carcinoma of the Head and Neck” OR “Head and Neck Squamous Cell Carcinoma” OR “HNSCC” OR “Carcinoma, Squamous Cell of Head and Neck” OR “Squamous Cell Carcinoma of the Larynx” OR “Laryngeal Squamous Cell Carcinoma” OR “Squamous Cell Carcinoma of Larynx” OR “Squamous Cell Carcinoma of the Nasal Cavity” OR “Oral Tongue Squamous Cell Carcinoma” OR “Hypopharyngeal Squamous Cell Carcinoma” OR “Oral Squamous Cell Carcinoma” OR “Oral Cavity Squamous Cell Carcinoma” OR “Oral Squamous Cell Carcinomas” OR “Squamous Cell Carcinoma of the Mouth” OR “Oropharyngeal Squamous Cell Carcinoma”) | 44,470 | |
| 3 | (#1) OR (#2) | 44470 | |
| 4 | “Human Papillomavirus Viruses”[Mesh] | 7628 | |
| 5 | (“Human Papillomavirus Viruses” OR “Human Papillomavirus Virus” OR “Papillomavirus Virus, Human” OR “Virus, Human Papillomavirus” OR “Human Papillomavirus” OR “Human Papillomaviruses” OR “HPV, Human Papillomavirus Viruses” OR “Human Papilloma Virus” OR “Human Papilloma Viruses” OR “Papilloma Virus, Human” OR “Virus, Human Papilloma” OR “HPV Human Papillomavirus” OR “HPV Human Papillomaviruses” OR “Human Papillomavirus, HPV” OR “Human Papillomaviruses, HPV” OR “HPV” OR “Wart virus”) | 67038 | |
| 6 | (#4) OR (#5) | 67038 | |
| 7 | (#3) AND (#6) | 5330 | |
| Embase | 1 | ‘head and neck squamous cell carcinomas’ OR ‘squamous cell carcinoma, head and neck’ OR ‘squamous cell carcinoma of the head and neck’ OR ‘head and neck squamous cell carcinoma’ OR ‘hnscc’ OR ‘carcinoma, squamous cell of head and neck’ OR ‘squamous cell carcinoma of the larynx’ OR ‘laryngeal squamous cell carcinoma’ OR ‘squamous cell carcinoma of larynx’ OR ‘squamous cell carcinoma of the nasal cavity’ OR ‘oral tongue squamous cell carcinoma’ OR ‘hypopharyngeal squamous cell carcinoma’ OR ‘oral squamous cell carcinoma’ OR ‘oral cavity squamous cell carcinoma’ OR ‘oral squamous cell carcinomas’ OR ‘squamous cell carcinoma of the mouth’ OR ‘oropharyngeal squamous cell carcinoma’ | 61774 |
| 2 | ‘human papillomavirus viruses’ OR ‘human papillomavirus virus’ OR ‘papillomavirus virus, human’ OR ‘virus, human papillomavirus’ OR ‘human papillomavirus’ OR ‘human papillomaviruses’ OR ‘hpv’ OR ‘hpv, human papillomavirus viruses’ OR ‘human papilloma virus’ OR ‘human papilloma viruses’ OR ‘papilloma virus, human’ OR ‘virus, human papilloma’ OR ‘hpv human papillomavirus’ OR ‘hpv human papillomaviruses’ OR ‘human papillomavirus, hpv’ OR ‘human papillomaviruses, hpv’ OR ‘wart virus’ OR ‘HPV’ | 100567 | |
| 3 | #1 AND #2 | 8646 | |
| Cochrane | 1 | MeSH descriptor: [Squamous Cell Carcinoma of Head and Neck] explode all trees | 485 |
| 2 | (Squamous Cell Carcinoma of Head and Neck):ti,ab,kw OR (Head And Neck Squamous Cell Carcinomas):ti,ab,kw OR (Squamous Cell Carcinoma, Head And Neck):ti,ab,kw OR (Squamous Cell Carcinoma of the Head and Neck):ti,ab,kw OR (Head and Neck Squamous Cell Carcinoma):ti,ab,kw | 3643 | |
| 3 | (HNSCC):ti,ab,kw OR (Carcinoma, Squamous Cell of Head and Neck):ti,ab,kw OR (Squamous Cell Carcinoma of the Larynx):ti,ab,kw OR (Laryngeal Squamous Cell Carcinoma):ti,ab,kw OR (Squamous Cell Carcinoma of Larynx):ti,ab,kw | 3850 | |
| 4 | (Squamous Cell Carcinoma of the Nasal Cavity):ti,ab,kw OR (Oral Tongue Squamous Cell Carcinoma):ti,ab,kw OR (Hypopharyngeal Squamous Cell Carcinoma):ti,ab,kw OR (Oral Squamous Cell Carcinoma):ti,ab,kw OR (Oral Cavity Squamous Cell Carcinoma):ti,ab,kw | 1862 | |
| 5 | (oral squamous-cell carcinomas):ti,ab,kw OR (Squamous Cell Carcinoma of the Mouth):ti,ab,kw OR (Oropharyngeal Squamous Cell Carcinoma):ti,ab,kw | 1300 | |
| 6 | #1 OR #2 OR #3 OR #4 OR #5 | 4697 | |
| 7 | MeSH descriptor: [Human Papillomavirus Viruses] explode all trees | 288 | |
| 8 | (Human Papillomavirus Viruses):ti,ab,kw OR (Human Papillomavirus Virus):ti,ab,kw OR (Papillomavirus Virus, Human):ti,ab,kw OR (Virus, Human Papillomavirus):ti,ab,kw OR (Human Papillomavirus):ti,ab,kw | 2797 | |
| 9 | (Human Papillomaviruses):ti,ab,kw OR (HPV, Human Papillomavirus Viruses):ti,ab,kw OR (Human Papilloma Virus):ti,ab,kw OR (Human Papilloma Viruses):ti,ab,kw OR (Papilloma Virus, Human):ti,ab,kw | 568 | |
| 10 | (Virus, Human Papilloma):ti,ab,kw OR (HPV Human Papillomavirus):ti,ab,kw OR (HPV Human Papillomaviruses):ti,ab,kw OR (Human Papillomavirus, HPV):ti,ab,kw OR (Human Papillomaviruses, HPV):ti,ab,kw | 2658 | |
| 11 | (HPV):ti,ab,kw OR (Wart virus):ti,ab,kw | 3953 | |
| 12 | #7 OR #8 OR #9 OR #10 OR #11 | 4367 | |
| 13 | #6 AND #12 | 481 | |
| Web of Science | 1 | TS=(Squamous Cell Carcinoma of Head and Neck) | 23490 |
| 2 | (((((((((((ALL=(Squamous Cell Carcinoma of Head and Neck)) OR ALL=(Head And Neck Squamous Cell Carcinomas)) OR ALL=(Squamous Cell Carcinoma of the Head and Neck)) OR ALL=(Squamous Cell Carcinoma of the Larynx)) OR ALL=(Laryngeal Squamous Cell Carcinoma)) OR ALL=(Squamous Cell Carcinoma of the Nasal Cavity)) OR ALL=(Oral Tongue Squamous Cell Carcinoma)) OR ALL=(Hypopharyngeal Squamous Cell Carcinoma)) OR ALL=(Oral Squamous Cell Carcinoma)) OR ALL=(Oral Cavity Squamous Cell Carcinoma)) OR ALL=(Squamous Cell Carcinoma of the Mouth)) OR ALL=(Oropharyngeal Squamous Cell Carcinoma) | 40954 | |
| 3 | #2 OR #1 | 40954 | |
| 4 | TS=(Human Papillomavirus Viruses) | 6505 | |
| 5 | ((((((((((((ALL=(Human Papillomavirus Viruses)) OR ALL=(Human Papillomavirus Virus)) OR ALL=(Papillomavirus Virus, Human)) OR ALL=(Virus, Human Papillomavirus)) OR ALL=(Human Papillomavirus)) OR ALL=(Human Papilloma Viruses)) OR ALL=(Papilloma Virus, Human)) OR ALL=(Virus, Human Papilloma)) OR ALL=(HPV Human Papillomavirus)) OR ALL=(HPV Human Papillomaviruses)) OR ALL=(Human Papillomavirus, HPV)) OR ALL=(HPV)) OR ALL=(Wart virus) | 40335 | |
| 6 | #4 OR #5 | 40189 | |
| 7 | #3 AND #6 | 7446 | |
| Search results | 21903 | ||
| duplicates removed | 8428 | ||
| Records remained | 14465 | ||
References
- Bray F, Laversanne M, Sung H. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. doi:https://doi.org/10.3322/caac.21834
- Sahin A, Gilligan T, Caudell J. Challenges with the 8th edition of the AJCC cancer staging manual for breast, testicular, and head and neck cancers. J Natl Compr Canc Netw. 2019;17:560-564. doi:https://doi.org/10.6004/jnccn.2019.5015
- Cmelak A, Arneson K, Chau N. Locally advanced head and neck cancer. Am Soc Clin Oncol Educ Book. Published online 2013:237-244. doi:https://doi.org/10.14694/EdBook_AM.2013.33.237
- Johnson D, Burtness B, Leemans C. Head and neck squamous cell carcinoma. Nat Rev Dis Primers. 2020;6. doi:https://doi.org/10.1038/s41572-020-00224-3
- Braakhuis B, Brakenhoff R, Leemans C. Treatment choice for locally advanced head and neck cancers on the basis of risk factors: biological risk factors. Ann Oncol. 2012;23:x173-177. doi:https://doi.org/10.1093/annonc/mds299
- Pfister D, Spencer S, Adelstein D. Head and Neck cancers, version 2.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2020;18:873-898. doi:https://doi.org/10.6004/jnccn.2020.0031
- Blanchard P, Baujat B, Holostenco V. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): a comprehensive analysis by tumour site. Radiother Oncol. 2011;100:33-40. doi:https://doi.org/10.1016/j.radonc.2011.05.036
- Pignon J, le Maître A, Maillard E. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol. 2009;92:4-14. doi:https://doi.org/10.1016/j.radonc.2009.04.014
- Lacas B, Carmel A, Landais C. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): An update on 107 randomized trials and 19,805 patients, on behalf of MACH-NC Group. Radiother Oncol. 2021;156:281-293. doi:https://doi.org/10.1016/j.radonc.2021.01.013
- Alfouzan A. Radiation therapy in head and neck cancer. Saudi Med J. 2021;42:247-254. doi:https://doi.org/10.15537/smj.2021.42.3.20210660
- Buglione M, Cavagnini R, Di Rosario F. Oral toxicity management in head and neck cancer patients treated with chemotherapy and radiation: Xerostomia and trismus (Part 2). Literature review and consensus statement. Crit Rev Oncol Hematol. 2016;102:47-54. doi:https://doi.org/10.1016/j.critrevonc.2016.03.012
- Cohen E, Karrison T, Kocherginsky M. Phase III randomized trial of induction chemotherapy in patients with N2 or N3 locally advanced head and neck cancer. J Clin Oncol. 2014;32:2735-2743. doi:https://doi.org/10.1200/jco.2013.54.6309
- Haddad R, O’Neill A, Rabinowits G. Induction chemotherapy followed by concurrent chemoradiotherapy (sequential chemoradiotherapy) versus concurrent chemoradiotherapy alone in locally advanced head and neck cancer (PARADIGM): a randomised phase 3 trial. Lancet Oncol. 2013;14:257-264. doi:https://doi.org/10.1016/s1470-2045(13)70011-1
- Li Q, Tie Y, Alu A. Targeted therapy for head and neck cancer: signaling pathways and clinical studies. Signal Transduct Target Ther. 2023;8. doi:https://doi.org/10.1038/s41392-022-01297-0
- Bonner J, Harari P, Giralt J. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21-28. doi:https://doi.org/10.1016/s1470-2045(09)70311-0
- Ang K, Zhang Q, Rosenthal D. Randomized phase III trial of concurrent accelerated radiation plus cisplatin with or without cetuximab for stage III to IV head and neck carcinoma: RTOG 0522. J Clin Oncol. 2014;32:2940-2950. doi:https://doi.org/10.1200/jco.2013.53.5633
- Seiwert T, Burtness B, Mehra R. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. 2016;17:956-965. doi:https://doi.org/10.1016/s1470-2045(16)30066-3
- Muzaffar J, Bari S, Kirtane K. Recent advances and future directions in clinical management of head and neck squamous cell carcinoma. Cancers (Basel). 2021;13. doi:https://doi.org/10.3390/cancers13020338
- Macha M, Wani N, Ganai R. Recent advances in head and neck tumor microenvironment-based therapy. Adv Exp Med Biol. 2020;1296:11-31. doi:https://doi.org/10.1007/978-3-030-59038-3_2
- Karbalaie Niya M, Safarnezhad Tameshkel F, Keyvani H. Epstein-Barr virus molecular epidemiology and variants identification in head and neck squamous cell carcinoma. Eur J Cancer Prev. 2020;29:523-530. doi:https://doi.org/10.1097/cej.0000000000000554
- Deng Z, Hasegawa M, Yamashita Y. Prognostic value of human papillomavirus and squamous cell carcinoma antigen in head and neck squamous cell carcinoma. Cancer Sci. 2012;103:2127-2134. doi:https://doi.org/10.1111/cas.12009
- Lechner M, Liu J, Masterson L. HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol. 2022;19:306-327. doi:https://doi.org/10.1038/s41571-022-00603-7
- Muñoz-Bello J, Romero-Córdoba S, García-Chávez J. Potential transcript-based biomarkers predicting clinical outcomes of HPV-positive head and neck squamous cell carcinoma patients. Cells. 2024;13. doi:https://doi.org/10.3390/cells13131107
- Gillison M, Chaturvedi A, Anderson W. Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol. 2015;33:3235-3242. doi:https://doi.org/10.1200/jco.2015.61.6995
- Bratman S, Bruce J, O’Sullivan B. Human papillomavirus genotype association with survival in head and neck squamous cell carcinoma. JAMA Oncol. 2016;2:823-826. doi:https://doi.org/10.1001/jamaoncol.2015.6587
- Di Credico G, Polesel J, Dal Maso L. Alcohol drinking and head and neck cancer risk: the joint effect of intensity and duration. Br J Cancer. 2020;123:1456-1463. doi:https://doi.org/10.1038/s41416-020-01031-z
- Di Credico G, Edefonti V, Polesel J. Joint effects of intensity and duration of cigarette smoking on the risk of head and neck cancer: a bivariate spline model approach. Oral Oncol. 2019;94:47-57. doi:https://doi.org/10.1016/j.oraloncology.2019.05.006
- Alsahafi E, Begg K, Amelio I. Clinical update on head and neck cancer: molecular biology and ongoing challenges. Cell Death Dis. 2019;10. doi:https://doi.org/10.1038/s41419-019-1769-9
- Amaral M, Faísca P, Ferreira H. Current insights and progress in the clinical management of head and neck cancer. Cancers (Basel). 2022;14. doi:https://doi.org/10.3390/cancers14246079
- Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6. doi:https://doi.org/10.1371/journal.pmed.1000097
- Cumpston M, Li T, Page M. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10. doi:https://doi.org/10.1002/14651858.Ed000142
- Guyot P, Ades A, Ouwens M. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12. doi:https://doi.org/10.1186/1471-2288-12-9
- Parmar M, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815-2834. doi:https://doi.org/10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8
- Harrington K, Berrier A, Robinson M. Randomised Phase II study of oral lapatinib combined with chemoradiotherapy in patients with advanced squamous cell carcinoma of the head and neck: rationale for future randomised trials in human papilloma virus-negative disease. Eur J Cancer. 2013;49:1609-1618. doi:https://doi.org/10.1016/j.ejca.2012.11.023
- Mesía R, Henke M, Fortin A. Chemoradiotherapy with or without panitumumab in patients with unresected, locally advanced squamous-cell carcinoma of the head and neck (CONCERT-1): a randomised, controlled, open-label phase 2 trial. Lancet Oncol. 2015;16:208-220. doi:https://doi.org/10.1016/s1470-2045(14)71198-2
- Strom T, Trotti A, Kish J. Comparison of every 3 week cisplatin or weekly cetuximab with concurrent radiotherapy for locally advanced head and neck cancer. Oral Oncol. 2015;51:704-708. doi:https://doi.org/10.1016/j.oraloncology.2015.04.012
- Tang C, Chan C, Jiang W. Concurrent cetuximab versus platinum-based chemoradiation for the definitive treatment of locoregionally advanced head and neck cancer. Head Neck. 2015;37:386-392. doi:https://doi.org/10.1002/hed.23609
- Nien H, Sturgis E, Kies M. Comparison of systemic therapies used concurrently with radiation for the treatment of human papillomavirus-associated oropharyngeal cancer. Head Neck. 2016;38:E1554-E1561. doi:https://doi.org/10.1002/hed.24278
- Ou D, Levy A, Blanchard P. Concurrent chemoradiotherapy with cisplatin or cetuximab for locally advanced head and neck squamous cell carcinomas: does human papilloma virus play a role?. Oral Oncol. 2016;59:50-57. doi:https://doi.org/10.1016/j.oraloncology.2016.05.019
- Rosenthal D, Harari P, Giralt J. Association of human papillomavirus and p16 status with outcomes in the IMCL-9815 Phase III registration trial for patients with locoregionally advanced oropharyngeal squamous cell carcinoma of the head and neck treated with radiotherapy with or without cetuximab. J Clin Oncol. 2016;34:1300-1308. doi:https://doi.org/10.1200/jco.2015.62.5970
- Adkins D, Ley J, Oppelt P. nab-Paclitaxel-based induction chemotherapy with or without cetuximab for locally advanced head and neck squamous cell carcinoma. Oral Oncol. 2017;72:26-31. doi:https://doi.org/10.1016/j.oraloncology.2017.07.001
- Buglione M, Maddalo M, Corvò R. Subgroup analysis according to human papillomavirus status and tumor site of a randomized phase II trial comparing cetuximab and cisplatin combined with radiation therapy for locally advanced head and neck cancer. Int J Radiat Oncol Biol Phys. 2017;97:462-472. doi:https://doi.org/10.1016/j.ijrobp.2016.10.011
- Barney C, Walston S, Zamora P. Clinical outcomes and prognostic factors in cisplatin versus cetuximab chemoradiation for locally advanced p16 positive oropharyngeal carcinoma. Oral Oncol. 2018;79:9-14. doi:https://doi.org/10.1016/j.oraloncology.2018.02.001
- Onita B, Lester D, Iman A. Comparison of high-dose cisplatin-based chemoradiotherapy and cetuximab-based bioradiotherapy for p16-positive oropharyngeal squamous cell carcinoma in the context of revised HPV-based staging. Rep Pract Oncol Radiother. 2018;23:451-457. doi:https://doi.org/10.1016/j.rpor.2018.08.007
- Gillison M, Trotti A, Harris J. Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet. 2019;393:40-50. doi:https://doi.org/10.1016/s0140-6736(18)32779-x
- Mehanna H, Robinson M, Hartley A. Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet. 2019;393:51-60. doi:https://doi.org/10.1016/s0140-6736(18)32752-1
- Patil V, Noronha V, Joshi A. A randomized phase 3 trial comparing nimotuzumab plus cisplatin chemoradiotherapy versus cisplatin chemoradiotherapy alone in locally advanced head and neck cancer. Cancer. 2019;125:3184-3197. doi:https://doi.org/10.1002/cncr.32179
- Beckham T, Barney C, Healy E. Platinum-based regimens versus cetuximab in definitive chemoradiation for human papillomavirus-unrelated head and neck cancer. Int J Cancer. 2020;147:107-115. doi:https://doi.org/10.1002/ijc.32736
- Jeong I, Mo H, Nguyen A. Primary chemoradiation with cisplatin versus cetuximab for locally advanced head and neck cancer: a retrospective cohort study. Exp Hematol Oncol. 2020;9. doi:https://doi.org/10.1186/s40164-020-00175-1
- Lee N, Ferris R, Psyrri A. Avelumab plus standard-of-care chemoradiotherapy versus chemoradiotherapy alone in patients with locally advanced squamous cell carcinoma of the head and neck: a randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Oncol. 2021;22:450-462. doi:https://doi.org/10.1016/s1470-2045(20)30737-3
- Rischin D, King M, Kenny L. Randomized trial of radiation therapy with weekly cisplatin or cetuximab in low-risk HPV-Associated Oropharyngeal Cancer (TROG 12.01) – A trans-tasman radiation oncology group study. Int J Radiat Oncol Biol Phys. 2021;111:876-886. doi:https://doi.org/10.1016/j.ijrobp.2021.04.015
- Yom S, Torres-Saavedra P, Caudell J. Reduced-dose radiation therapy for HPV – associated oropharyngeal carcinoma (NRG Oncology HN002). J Clin Oncol. 2021;39:956-965. doi:https://doi.org/10.1200/jco.20.03128
- Wong S, Torres-Saavedra P, Saba N. Radiotherapy plus cisplatin with or without lapatinib for non-human papillomavirus head and neck carcinoma: a Phase 2 randomized clinical trial. JAMA Oncol. 2023;9:1565-1573. doi:https://doi.org/10.1001/jamaoncol.2023.3809
- Sher D, Schwartz D, Nedzi L. Comparative effectiveness of induction chemotherapy for oropharyngeal squamous cell carcinoma: a population-based analysis. Oral Oncol. 2016;54:58-67. doi:https://doi.org/10.1016/j.oraloncology.2015.12.008
- Bhattasali O, Han J, Thompson L. Induction chemotherapy followed by concurrent chemoradiation versus concurrent chemoradiation alone in the definitive management of p16-positive oropharyngeal squamous cell carcinoma with low-neck or N3 disease. Oral Oncol. 2018;78:151-155. doi:https://doi.org/10.1016/j.oraloncology.2018.01.031
- Lorch J, Hanna G, Posner M. Human papillomavirus and induction chemotherapy versus concurrent chemoradiotherapy in locally advanced oropharyngeal cancer: the Dana Farber Experience. Head Neck. 2016;38:E1618-E1624. doi:https://doi.org/10.1002/hed.24289
- Dobrosotskaya I, Bellile E, Spector M. Weekly chemotherapy with radiation versus high-dose cisplatin with radiation as organ preservation for patients with HPV-positive and HPV-negative locally advanced squamous cell carcinoma of the oropharynx. Head Neck. 2014;36:617-623. doi:https://doi.org/10.1002/hed.23339
- Mercke C, Wickart-Johansson G, Sjödin H. Radiotherapy-dose escalated for large volume primary tumors-and cetuximab with or without induction chemotherapy for HPV associated squamous cell carcinoma of the head and neck – A randomized Phase II trial. Cancers (Basel). 2023;15. doi:https://doi.org/10.3390/cancers15092543
- Geoffrois L, Martin L, De Raucourt D. Induction chemotherapy followed by cetuximab radiotherapy is not superior to concurrent chemoradiotherapy for head and neck carcinomas: results of the GORTEC 2007-02 Phase III randomized trial. J Clin Oncol. 2018;36:3077-3083. doi:https://doi.org/10.1200/jco.2017.76.2591
- Голубев П, Болотина Л, Геворков А. Эффективность двухкомпонентного режима индукционной химиотерапии при лечении ВПЧ-позитивного плоскоклеточного рака ротоглотки. Сибирский онкологический журнал. 2023;22:26-33. doi:https://doi.org/10.21294/1814-4861-2023-22-2-26-33
- Hall S, Griffiths R, O’Sullivan B. The addition of chemotherapy to radiotherapy did not reduce the rate of distant metastases in low-risk HPV-related oropharyngeal cancer in a real-world setting. Head Neck. 2019;41:2271-2276. doi:https://doi.org/10.1002/hed.25679
- Burtness B, Haddad R, Dinis J. Afatinib vs placebo as adjuvant therapy after chemoradiotherapy in squamous cell carcinoma of the head and neck: a randomized clinical trial. JAMA Oncol. 2019;5:1170-1180. doi:https://doi.org/10.1001/jamaoncol.2019.1146
- De Felice F, Abate G, Galdieri A. Impact of induction chemotherapy in locally advanced HPV-negative oropharyngeal cancer. A propensity score-matched analysis. Anticancer Res. 2016;36:6667-6672. doi:https://doi.org/10.21873/anticanres.11276
- Riaz N, Sherman E, Koutcher L. Concurrent chemoradiotherapy with cisplatin versus cetuximab for squamous cell carcinoma of the head and neck. Am J Clin Oncol. 2016;39:27-31. doi:https://doi.org/10.1097/coc.0000000000000006
- Hammerman P, Hayes D, Grandis J. Therapeutic insights from genomic studies of head and neck squamous cell carcinomas. Cancer Discov. 2015;5:239-244. doi:https://doi.org/10.1158/2159-8290.Cd-14-1205
- Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature. 2015;517:576-582. doi:https://doi.org/10.1038/nature14129
- Agrawal N, Frederick M, Pickering C. Exome sequencing of head and neck squamous cell carcinoma reveals inactivating mutations in NOTCH1. Science. 2011;333:1154-1157. doi:https://doi.org/10.1126/science.1206923
- Stransky N, Egloff A, Tward A. The mutational landscape of head and neck squamous cell carcinoma. Science. 2011;333:1157-1160. doi:https://doi.org/10.1126/science.1208130
- Fung N, Faraji F, Kang H. The role of human papillomavirus on the prognosis and treatment of oropharyngeal carcinoma. Cancer Metastasis Rev. 2017;36:449-461. doi:https://doi.org/10.1007/s10555-017-9686-9
- Blitzer G, Smith M, Harris S. Review of the clinical and biologic aspects of human papillomavirus-positive squamous cell carcinomas of the head and neck. Int J Radiat Oncol Biol Phys. 2014;88:761-770. doi:https://doi.org/10.1016/j.ijrobp.2013.08.029
- Vermeer D, Spanos W, Vermeer P. Radiation-induced loss of cell surface CD47 enhances immune-mediated clearance of human papillomavirus-positive cancer. Int J Cancer. 2013;133:120-129. doi:https://doi.org/10.1002/ijc.28015
- Vu H, Sikora A, Fu S. HPV-induced oropharyngeal cancer, immune response and response to therapy. Cancer Lett. 2010;288:149-155. doi:https://doi.org/10.1016/j.canlet.2009.06.026
- Elhalawani H, Mohamed A, Elgohari B. Tobacco exposure as a major modifier of oncologic outcomes in human papillomavirus (HPV) associated oropharyngeal squamous cell carcinoma. BMC Cancer. 2020;20. doi:https://doi.org/10.1186/s12885-020-07427-7
- Tagliabue M, Mena M, Maffini F. Role of human papillomavirus infection in head and neck cancer in Italy: the HPV-AHEAD study. Cancers (Basel). 2020;12. doi:https://doi.org/10.3390/cancers12123567
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1060 times
- PDF downloaded - 95 times



