Reviews
Vol. 45: Issue 6 - December 2025
The nature of nasal discharge in chronic rhinosinusitis: a systematic review and meta-analysis using patientreported outcomes
Reviewing Nasal Discharge in CRS
Abstract
Objective. The objective of this study is to answer the question “What is the most common and severe type of nasal discharge in patients with chronic rhinosinusitis (CRS) at baseline as measured by patient-reported outcomes?”.
Methodology. Two independent reviewers evaluated studies for inclusion, extracted data from included studies, and performed critical appraisal of studies. Data on the four Sino-Nasal Outcome Test 22 (SNOT22) discharge questions, demographic, and comorbidity data was collected. Meta-analysis of single means and proportions was performed for demographic, comorbidity, severity, and prevalence data.
Results. A total of 53 studies (n = 6584) were included for analysis. Postnasal drip (PND) was the most severe symptom (2.6, 95%CI: 2.2-3) and most prevalent (80.7%, 95%CI: 53.0-97.7). Patients without nasal polyps had a higher PND score than those with polyps (2.56 vs 2.40, 95%CI: 0.1-0.2). However, patients with polyps reported higher symptom scores for need to blow nose, runny nose, and thick nasal discharge (all p < 0.0001).
Conclusions. CRS patients experience PND at a higher prevalence and severity at baseline than the other three forms of nasal discharge captured by the SNOT22. Polyp status influences differing symptoms of nasal drainage. Comorbid asthma or allergies are associated with more severe PND and total SNOT22 scores.
Introduction
Chronic rhinosinusitis (CRS) has a high prevalence and morbidity in the United States and internationally 1. The diagnosis of CRS requires two or more of the following cardinal symptoms: nasal discharge, nasal obstruction, hyposmia, and facial pain or pressure, with at least one being nasal discharge or obstruction 1. The Sino-Nasal Outcome Test (SNOT) is a highly validated and widely used tool to characterise quality of life in CRS 2. The SNOT22 captures nasal discharge in four ways: “need to blow nose”, “runny nose”, “postnasal discharge” (PND), and “thick nasal discharge” 3. Nasal discharge is widely prevalent in patients with CRS, as 51 to 83% of patients report its presence 1. Nasal discharge is considered highly burdensome by most CRS patients, with 77% marking “need to blow nose” as “important” on the SNOT22, followed by thick nasal discharge (71%), PND (70%), and runny nose (57%) 4.
While the other three cardinal symptoms are represented by a single question on the SNOT22, discharge requires four unique questions. Patients often describe discharge symptoms as “congestion”, which can be confused with separate symptoms such as nasal obstruction or facial pressure 5,6. The setting in which discharge presents is often further obscured by comorbid conditions such as asthma, allergies, and gastro-oesophageal reflux disease, as all three can affect the upper airway 7,8. These comorbidities impact treatment plans and likelihood for symptom improvement; thus, they are important considerations when counselling patients.
While there are meta-analyses investigating patient reported outcomes in CRS, there are no studies specifically evaluating nasal discharge. This paucity of literature is highlighted by studies evaluating the clinical burden of other cardinal symptoms of CRS, such as facial pressure 9. This study seeks to bolster the current understanding of CRS cardinal symptoms by characterising nasal discharge. Understanding the overall burden of CRS is important; however, patients often think of their disease in terms of specific symptoms. By characterising the presentation of a single cardinal symptom of CRS, this study will help inform providers on how to offer a unified, mutually understood dialogue and personalised counselling to patients experiencing discharge. The goal of this systematic review and meta-analysis is to quantify the prevalence and severity of each of the four nasal discharge questions on the SNOT22 in adults with CRS. The authors hypothesised that there will be differences in both the prevalence and severity of the four nasal discharge symptoms, particularly when stratifying by various comorbidities.
Materials and methods
Search criteria
This systematic review was conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) criteria 10. The PICOTS question guiding this systematic review is “What is the prevalence and severity of baseline nasal discharge symptoms in adults with CRS?” A broad-scoping literature search was conducted on June 10th, 2024 using Cochrane library, PubMed (National Library of Medicine), Scopus (Elsevier), and CINAHL (EBSCO). A literature search designed for PubMed included keywords and medical subjected headings (MeSH) related to CRS, SNOT22, and nasal discharge. The PubMed search strategy was applied to Cochrane, Scopus and CINAHL. The Scopus search was limited to medicine (subject), articles (document), final (publication status), humans (keyword), journal (source type), and English (language). No filters were applied to PubMed, Cochrane, or CINAHL. Once the literature search was completed, articles were uploaded to Covidence systematic review software.
Study selection
Two authors (ATR and EEB) independently screened articles for inclusion by title and abstract first, followed by full text review. Discrepancies between reviewers were resolved by a third party (EMK). Inclusion criteria were 1) diagnosis of CRS and 2) itemised survey data regarding nasal discharge from SNOT20, SNOT22, or Visual Analogue Scale (VAS) questionnaires. Exclusion criteria were 1) animal studies, 2) studies without available English translation, 3) case studies, 4) review articles, 5) non-itemised questionnaire data, 6) non-extractable data, 7) non-exclusive CRS population, 8) studies post-surgical or medical intervention, and 9) paediatric population < 16 years of age.
Study appraisal
Each study was assigned a level of evidence according to the Oxford Centre for Evidence-Based Medicine criteria 11. Randomised control trials were assessed for risk of bias via the Revised Cochrane risk-of-bias tool for randomised trials (RoB-2), while non-randomised studies were assessed for risk of bias with the Risk of Bias in Non-Randomized Studies – of Interventions (ROBINS-I) assessment tool 12,13. Case series, cross-sectional, and case-control studies were assessed for risk of bias using the Joanna Briggs Institute (JBI) Critical Appraisal Tool checklist 14. Two authors (EMK and IVS) independently assessed each study using a checklist, and all conflicting answers were reconciled by a third party (SAN). For studies using the RoB-2 and ROBINS-I assessment, response options included “low risk,” “high risk” or “unclear.” For studies in which the JBI was utilised, each item was given a score of “1” for “yes” and “0” for “no,” “not applicable,” or “unclear.” The case series and case control checklists have 10 questions and were scored out of 10. A score of 5 or higher on either checklist was considered at low risk for bias. Cross-sectional checklists have 8 questions and were scored out of 8. A score of 4 or higher was considered at low risk for bias. Only studies classified as low risk for bias were included in the final analysis.
Data extraction
Two authors (ATR and EEB) independently extracted data into a standardised spreadsheet. Any conflicts or inaccuracies were resolved by a third party (EMK). Extracted data included author name, year of publication, sample size, study population, demographics, comorbidities, and intervention. Outcome data included total SNOT score, and itemised SNOT or VAS scores for any nasal discharge symptom. VAS scores were standardised to a 0-100 cm scale to improve consistency in measurements. Due to variation in VAS reporting, the following terms were equated to nasal discharge: “nasal secretion”, “sticky secretion”, “purulent rhinorrhoea”, “purulence”, and “discharge”. The terms “runny nose”, and “anterior rhinorrhoea” were categorised as rhinorrhoea. Conversely, “posterior rhinorrhoea” was classified as postnasal drip. The authors were able to obtain patient level data on adults with chronic rhinosinusitis from a longitudinal study discussed in Mattos et al. 4. These data included patient demographic information, prior therapy attempted, comorbid diagnoses, and itemised baseline SNOT22 scores. The extraction process involved objective and clearly defined criteria, which minimised the potential for subjective interpretation by the reviewers. Therefore, no formal interrater reliability statistics (e.g., Cohen’s Kappa) were calculated.
Statistical analysis
Meta-analysis of single means (age, symptom duration, body mass index [BMI], SNOT22 scores, VAS scores) and meta-analysis of proportions (gender, comorbidities, patient characteristics, prevalence of SNOT symptoms, prevalence of VAS symptoms) were performed by Comprehensive Meta-Analysis version 4 (Biostat Inc., Englewood, NJ, USA). Each measure (mean/proportion and 95% confidence interval [CI]) was weighted according to the number of patients affected. As some studies reported the outcomes in median (first quartile, third quartile), the quantile estimation (QE) method as specified by Cochrane Review was deployed to calculate the pooled estimates 15-17. Heterogeneity among studies was assessed using I-squared (I2) statistics with fixed effects (I2 < 50%) and random effects (I2 > 50%). To assess the robustness of our findings, we performed a sensitivity analysis using the one-study removal technique, which systematically excludes one study at a time to evaluate the impact of individual studies on the pooled results. In addition, a comparison of means and proportions, expressed as difference (Δ) and 95% CI was done to compare outcomes between two groups. Finally, potential publication bias was evaluated by visual inspection of the funnel plot and Egger’s regression test, which statistically examines the asymmetry of the funnel plot 18,19. A p value of < 0.05 was considered to indicate a significant difference for all statistical tests.
Results
Search results and study characteristics
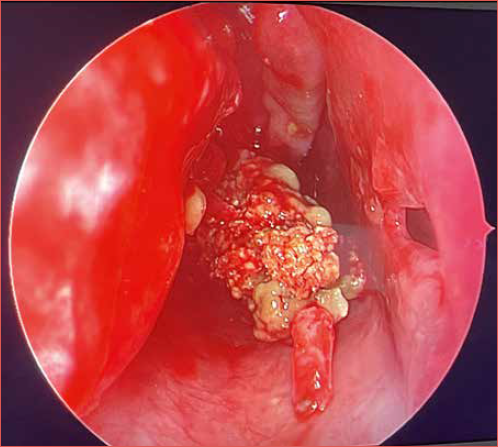
The literature search yielded 1628 studies, of which 252 duplicates were removed. 1376 articles underwent title and abstract screening. Full text review was performed on 403 studies and 350 studies were excluded. Reasons for exclusion included wrong outcomes, no SNOT score, no individual component SNOT scores, wrong population, improper study design, non-English text, unavailable full text, and concern for bias. At the conclusion of the review, 53 articles met the inclusion criteria 20-68. A PRISMA diagram detailing the systematic review is provided in Figure 1. The most common grounds for exclusion were wrong outcomes; either no SNOT22 score or no itemised SNOT22 scores for nasal discharge. A summary of the studies included is provided in Table I.
Studies included for analysis were published between 2002 and 2024. Descriptive features of included studies are listed in Table I. Critical appraisal of studies indicated an acceptably low risk of bias for all studies included. Potential sources of bias were most pronounced with confounding, missing data, classification of interventions, and selective reporting in the non-randomised studies (Fig. 2). All randomised studies were considered low risk, the greatest sources of potential bias were observed in the randomisation process and in deviations from study protocol. JBI assessment also found a low risk of bias for cross-sectional, case series, and case-control studies, all having scores higher than 4, 5, or 5, for each respective study design.
ROBINS-I Risk of BiasA funnel plot with Egger’s test, -0.11 ([95% CI: -1.4-1.2], p = 0.86), showed that 49 of 53 studies were within the funnel plot with little asymmetry, suggesting low potential for publication bias (Fig. 3). This suggests a low likelihood that studies included in this analysis were more likely to publish significant results compared to non-significant results.
Patient characteristics
A total of 7193 patients with CRS were included with a mean age of 45.9 (range: 16-94; 95% CI: 44-48.1). Slightly over half the study population was male. The study population had a notably higher rate of nasal polyposis than the overall CRS population. This could be due to the inclusion of studies that selected specifically for CRS with nasal polyps (CRSwNP). Cystic fibrosis was also overrepresented as one study included exclusively these patients. Additional characteristics and comorbidities of the CRS group are provided in Table II.
Severity of symptoms
Data comparing the severity of SNOT and VAS nasal discharge symptoms in CRS patients, including data stratified by polyp status and comorbidities, are provided in Table III. Across all studies, “post-nasal drip” (PND) was the SNOT-22 symptom score reported with highest severity (2.60) in patients with CRS. This was significantly higher than “need to blow nose” at 2.50, “runny nose” at 2.44, and “thick nasal discharge” at 2.32 ([95% CIs: 0.09-0.11, 0.15-0.17, and 0.27-0.29, respectively], all p < 0.0001). While these differences are statistically significant, they do not meet the threshold for clinical significance (0.8) 69. VAS “nasal discharge”, “post-nasal drip” and “rhinorrhoea” were 54.3, 57.2 and 57.3, respectively. VAS “rhinorrhoea” and “post-nasal drip” were both significantly higher than “nasal discharge” ([95% CIs: 2.8-3.1 and 2.8-3, respectively], both p < 0.0001); however, no significant difference exists between the two ([95% CI: -0.04-0.3], p = 0.16).
When comparing CRS subtypes, patients without polyps (CRSsNP) reported significantly higher PND scores than patients with polyps (2.56 vs 2.40, 95% CI 0.12-0.20, p < 0.0001). However, patients with polyps (CRSwNP) reported significantly higher scores for need to blow nose, runny nose, and thick nasal discharge ([95% CIs: 0.7-0.8, 0.8-0.9, and 0.2-0.3], all p < 0.0001). Patients with comorbid asthma reported PND 3.1 and thick nasal discharge 3.1 as the most severe. Those with allergies also reported PND as most severe.
Prevalence of symptoms
On a scale from 0-5, the most frequently reported score for PND was 4. The other three nasal discharge symptoms were most frequently reported with a score of 3. Figure 4 describes the total distribution for each nasal discharge symptom. The distribution of scores was stratified into “mild” for 0-2 and “severe” for 3-5. This stratification was based upon what the authors considered a natural break in the distribution of nasal discharge scores reported in Figure 4. In the overall cohort, PND had the highest proportion of severe scores at 67.3% of patients, followed by thick nasal discharge (65%), need to blow nose (61.6%), and runny nose (48.5%).
Figure 5 describes the percentage of patients reporting severe symptoms by polyp status, with asthma, and with allergies. Patients without polyps more frequently reported severe PND compared to those with polyps (71 vs 63% [95% CI: 2.2-13.6]). However, the CRSwNP group more frequently reported severe scores for the other three nasal discharge symptoms. Patients with comorbid asthma and allergies also reported severe PND in high proportions, at 70% and 72%, respectively.
Discussion
Nasal discharge is one of the four cardinal symptoms used to diagnose CRS and affects up to 83% of patients 1. There are various ways that patients can describe nasal discharge, which can obscure a clinician’s understanding of their disease burden 6. This picture can be further distorted by patient-specific comorbidities. For example, it may not be readily clear in an atopic patient if rhinorrhoea is due to their allergies, their sinus disease, or a mixture of both. Dysphonia may be attributed to PND when in reality it is caused by laryngopharyngeal reflux. A nuanced understanding of how these comorbidities affect nasal discharge reporting on the SNOT22 is important, as it can help providers determine the true source of symptoms, guide treatment plans, and allow for better patient counselling.
Nasal discharge can be divided into two categories; anterior and posterior 1. Across all studies, patients reported PND as the most severe discharge symptom on the SNOT22, followed by need to blow nose, runny nose, and thick nasal discharge, respectively. While need to blow nose and thick nasal discharge do not fit specifically into anterior or posterior, the difference between postnasal discharge and runny nose suggests that PND may be more closely associated with severe CRS.
Further analysis by CRS subtypes and comorbidities presented a similar pattern. PND was the most severe symptom for patients without nasal polyps and for patients with comorbid asthma and allergies. However, this was not the case for patients with nasal polyps, who reported need to blow nose as the most severe symptom. In fact, the severity of PND for polyp patients was significantly lower than that of patients without polyps. Runny nose was also more severe than PND in patients with nasal polyps. In contrast with the rest of the study population, it appears that higher scores for anterior nasal symptoms are associated with nasal polyposis.
An interesting finding from this study is the severe nasal discharge observed in patients with asthma. While total SNOT22 takes into account many systemic symptoms that may be impacted by asthma, such as fatigue, cough, and impact upon sleep, it is surprising that it also appears to result in more severe nasal drainage symptoms. Patients with comorbid allergies also reported severe PND; however, there were not significant differences in nasal discharge symptoms between comorbid asthma and allergy groups. Interestingly, the asthma group had a more severe baseline presentation than the allergy group, as illustrated by a significantly higher total SNOT22 score.
There is a well-established association between CRS and asthma, with 25% of CRS patients having a diagnosis of asthma compared to 5% of the general population 1. Within CRS, there has been a more specific association between nasal polyposis and asthma. The current understanding is that Type 2 (T2) inflammation is a mediator for both diseases, using IL-5 and IL-13 to promote eosinophilia 70. A recent study found that 62% of patients with nasal polyps have solely T2 inflammation mediating their disease, and 87% of these patients have T2 inflammation present in some capacity 70. Patients across all CRS subtypes with T2 inflammation were significantly more likely to also have a diagnosis of polyps and asthma compared to the T1 and T3 inflammation types 70.
The mechanism behind severe discharge in asthma is not entirely clear. Our main hypothesis is that patients with comorbid asthma are more likely to have a higher overall burden of inflammation, which can worsen nasal symptoms. This is in line with the “unified airway” concept, which postulates that the diseases of the upper and lower airway can affect both areas due to similar anatomy, immune defense mechanisms, and exposures 1. A recent study comparing asthma severity and SNOT22 questions found a strong correlation between poor asthma control and more severe postnasal discharge scores 71. The same study examined nasal symptoms in patients who had recently visited the emergency department for asthma exacerbations. In this group, authors observed higher total SNOT22 scores and runny nose scores compared to patients who had not sought emergency care 71. While these results were not stratified by polyp status, both associations support the idea that poorly controlled inflammation in the lower airway can have negative effects on the upper airway. This concept is important when creating a holistic treatment plan for patients, as upper airway symptoms might not resolve if treatment does not include therapy directed at their lower airway pathologies.
A strength of this review is that we included all available studies to quantify the prevalence and severity of each of the four nasal discharge questions on the SNOT22 in adults with CRS. There are several limitations that should still be considered. First, as demonstrated by Fischer et al., patients often describe their symptoms in ways that vary from providers 6. While the SNOT22 attempts to characterise nasal discharge in four distinct ways, patients may think of their symptoms differently and struggle to place them within one of these domains. Second, the majority of studies investigating nasal discharge report SNOT22 data either in total score only or as a rhinologic domain, which accounts for the scores of all 7 nasal questions. Thus, the number of studies that included itemised SNOT22 data was limited in relation to the total body of literature regarding nasal discharge.
Discrete patient data was limited in the studies included, which posed difficulties in our subgroup analysis. Additionally, it was not feasible to completely account for overlap that may occur between polyp status and diagnosis of asthma or allergies. These limitations highlight the challenges posed by the availability of data and the rarity of certain outcomes in the studies included. Future studies should attempt to further stratify these data to analyse the individual effect that each of these diseases has on nasal discharge.
This stratified analysis can be used to personalise a clinician’s approach to managing the symptoms of nasal discharge in CRS. The findings presented show that there is variability in the prevalence and severity of the four types of nasal discharge captured by the SNOT22. The results of this study also illustrate how comorbidities and CRS subtype can associate with nasal discharge presentation. A personalised approach to clinical care can consider how patients experience each of the four symptoms and incorporate management of comorbidities with CRS treatment.
Conclusions
Our findings suggest that patients with CRS tend to report postnasal discharge as the most severe nasal discharge symptom on the SNOT22. Patients without nasal polyps experience more severe PND. Comorbid asthma may be a factor that worsens PND, both in patients with and without nasal polyps. Consideration of individual SNOT22 items, in addition to overall score, can enable clinicians to tailor their approach to each patient.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
EMK, ATR, EEB: data curation, formal analysis, writing; SAN: formal analysis, writing (review), supervision; AND, TLS, ZMS: writing (review); IVS – data curation; JCM: data curation, writing (review); RJS: conceptualization, supervision, writing (review).
Ethical consideration
Not applicable.
History
Received: April 23, 2025
Accepted: June 10, 2025
Figures and tables
Figure 1. PRISMA systematic review flow diagram.
Figure 2. ROBINS-I risk of biasA funnel plot with Egger’s test.
Figure 3. Funnel plot for publication bias.
Figure 4. SNOT22 score distribution in adults with CRS.
Figure 5. Proportion of patients reporting severe symptoms (score 3-5).
| Author, yr | OLE | Patients (n) | Male (n) | Age in years, mean (range) | CRSwNP/CRSsNP (n) | Outcomes |
|---|---|---|---|---|---|---|
| Alicandri-Ciufelli, 2024 | 2 | 145 | 89 | 55.1 (27-86) | 145/0 | SNOT, VAS |
| Anushivari, 2018 | 2 | 39 | - | - | - | SNOT |
| Bachert, 2017 | 2 | 105 | 75 | 50.5 | 105/0 | SNOT, VAS |
| Byun, 2013 | 2 | 25 | 18 | 49.9 (18-77) | 25/0 | SNOT, VAS |
| Cervin, 2002 | 4 | 17 | - | (18-67) | - | VAS |
| Chen, 2016 | 3 | 42 | - | 45.9 | 10/0 | VAS |
| Dabirmoghaddam, 2013 | 4 | 43 | 23 | 40.7 (17-64) | 40/0 | VAS |
| Deconde, 2014 | 3 | 339 | 151 | 51 | 123/216 | SNOT |
| De Corso, 2023 | 4 | 648 | 400 | 54 | 648/0 | SNOT, VAS |
| De Corso, 2024 | 3 | 101 | 60 | 46.8 | 101/0 | SNOT, VAS |
| Ebbens, 2006 | 2 | 116 | 77 | 46.8 | 95/21 | VAS |
| Gelardi, 2022 | 2 | 330 | 202 | 52.1 | 330/0 | SNOT |
| Ghadersohi 2020 | 3 | 51 | - | - | 21/30 | SNOT |
| Greguric, 2016 | 4 | 117 | 57 | 44.5 | 0/117 | SNOT, VAS |
| Guo, 2024 | 4 | 87 | 54 | 42.5 | 87/0 | SNOT, VAS |
| Hao, 2022 | 4 | 106 | 83 | 49.3 | 106/0 | SNOT, VAS |
| Huang, 2019 | 3 | 60 | 39 | 37.6 | - | SNOT, VAS |
| Jamtoy, 2021 | 4 | 10 | 7 | 47.3 (18-70) | 10/0 | SNOT, VAS |
| Ji, 2019 | 4 | 124 | 67 | 50.4 | - | SNOT |
| Lal, 2016 | 4 | 272 | 140 | 54.6 | 141/131 | SNOT |
| Ling - AJRA, 2007 | 4 | 201 | 104 | 49 (18-80) | - | SNOT, VAS |
| Ling - Laryngoscope, 2007 | 2 | 158 | 85 | 49.4 (18-80) | - | VAS |
| Liu, 2024 | 2 | 69 | 44 | 34.6 | 36/33 | SNOT |
| Liu, Gardner, 2023 | 4 | 115 | 47 | 50.6 | 0/115 | SNOT |
| Liu, Woodworth, 2023 | 4 | 105 | 44 | 53.7 | 0/105 | SNOT |
| Lourijsen, 2022 | 2 | 234 | 142 | 50.5 | 234/0 | SNOT |
| Mattos, 2019 | 3 | 100 | 54 | 54.7 | 59/41 | SNOT |
| Nabavi, 2023 | 2 | 90 | 41 | 41.1 | 90/0 | SNOT, VAS |
| Nguyen, 2017 | 4 | 63 | 32 | 51 | 63/0 | VAS |
| Niknami, 2021 | 2 | 100 | 60 | 37.4 (17-60) | - | VAS |
| Pacaci Cetin, 2024 | 4 | 28 | 12 | 46.6 (21-70) | 28/0 | SNOT, VAS |
| Pan, 2021 | 2 | 298 | 190 | 44 | - | VAS |
| Paoletti, 2023 | 4 | 33 | 13 | 54.2 | 33/0 | SNOT |
| Penezic, 2020 | 2 | 250 | 123 | 45.6 | 97/0 | SNOT |
| Pham, 2023 | 2 | 62 | 27 | 45.1 | 13/0 | SNOT |
| Qi, 2021 | 3 | 56 | 30 | 46.3 (18-78) | 56/0 | VAS |
| Salama, 2009 | 4 | 143 | - | 85/56 | VAS | |
| Savietto, 2020 | 2 | 30 | 15 | (18-65) | 0/30 | SNOT, VAS |
| Shao, 2023 | 4 | 32 | 11 | 40.9 | 32/0 | VAS |
| Sima, 2023 | 3 | 44 | 22 | 45.3 | 44/0 | SNOT, VAS |
| Soler, 2008 | 3 | 275 | 113 | 44.4 | 91/184 | VAS |
| Stolovitzky, 2019 | 2 | 400 | 243 | 49.6 | 400/0 | VAS |
| Suh, 2012 | 3 | 11 | 8 | 53.0 (32-70) | 11/0 | SNOT |
| Tat, 2022 | 4 | 17 | 8 | 41.9 | 17/0 | SNOT, VAS |
| Thunberg., 2020 | 2 | 34 | 12 | 52 (34-77) | 18/16 | VAS |
| Tiotiu, 2002 | 4 | 24 | 14 | 49 | 24/0 | VAS |
| Tomljenovic, 2014 | 2 | 32 | 11 | 43.6 (23-65) | 0/32 | SNOT, VAS |
| Verma, 2022 | 4 | 40 | 24 | 40.5 | 25/15 | SNOT, VAS |
| Xu, 2020 | 2 | 99 | 62 | 40.2 | 99/0 | VAS |
| Young, 2007 | 4 | 82 | 43 | 47.5 (26-77) | - | VAS |
| Yu, 2022 | 2 | 502 | 338 | 46 | 502/0 | VAS |
| Zeng, 2011 | 2 | 43 | 29 | 32.6 | 0/43 | VAS |
| Zhou, 2023 | 2 | 49 | 30 | 39.8 (18-67) | 49/0 | VAS |
| OLE: Oxford level of evidence; CRSwNP: chronic rhinosinusitis with nasal polyps; CRSsNP: chronic rhinosinusitis without nasal polyps; SNOT: study provides data from SNOT22; VAS: study provides data using the visual analog scale. | ||||||
| CRS patient characteristics | Proportion (%) | 95% CI |
|---|---|---|
| CRSwNP | 78.8 | 65.5-89.6 |
| CRSsNP | 20.4 | 9.9-33.5 |
| Asthma | 54.7 | 47.2-62.2 |
| Allergy | 50.1 | 38.2-61.9 |
| AERD/ASA sensitivity* | 26.8 | 22.1-31.8 |
| AFRS* | 25.1 | 7.3-49 |
| CF* | 59.3 | 12.3-73.1 |
| GERD | 6.5 | 0.56-18.3 |
| Smoking history | 30.7 | 20.3-42.3 |
| Prior surgery | 76 | 63-86.9 |
| CRS: chronic rhinosinusitis; CI: confidence interval; CRSwNP: chronic rhinosinusitis with nasal polyps; CRSsNP: chronic rhinosinusitis without nasal polyps; AERD: aspirin exacerbated respiratory disease; ASA: aspirin; AFRS: allergic fungal rhinosinusitis; CF: cystic fibrosis; GERD: gastro-oesophageal reflux disease. *These proportion calculations were among the CRSwNP study population, not the entire study population. | ||
| Metric | Group | Total patients | Mean score | 95% CI |
|---|---|---|---|---|
| Total SNOT Score | Overall | 4803 | 45.7 | 42.1-49.2 |
| CRSwNP | 2456 | 51.4** | 45.9-56.8 | |
| CRSsNP | 973 | 42.1 | 36.7-47.5 | |
| Asthma | 521 | 59.9 | 41.5-78.5 | |
| Allergy | 534 | 50.9 | 47-54.8 | |
| SNOT Need to Blow Nose | Overall | 2266 | 2.5 | 2.3-2.7 |
| CRSwNP | 783 | 3** | 2.9-3.1 | |
| CRSsNP | 826 | 2.3 | 2-2.5 | |
| Asthma | 424 | 2.9 | 2.8-3 | |
| Allergy | 492 | 2.8 | 2.7-2.9 | |
| SNOT Runny Nose | Overall | 2266 | 2.4 | 2.2-2.7 |
| CRSwNP | 783 | 2.8** | 2.5-3.2 | |
| CRSsNP | 826 | 2 | 1.8-2.2 | |
| Asthma | 424 | 2.5 | 2.4-2.7 | |
| Allergy | 492 | 2.4 | 2.3-2.6 | |
| SNOT Postnasal Drip | Overall | 2266 | 2.6 | 2.2-3 |
| CRSwNP | 783 | 2.4 | 1.6-3.2 | |
| CRSsNP | 826 | 2.6* | 1.9-3.2 | |
| Asthma | 424 | 3.1 | 3-3.2 | |
| Allergy | 492 | 3.1 | 3-3.3 | |
| SNOTThick Nasal Discharge | Overall | 2266 | 2.3 | 2.1-2.6 |
| CRSwNP | 783 | 2.5** | 1.5-3.5 | |
| CRSsNP | 826 | 2.3 | 1.7-2.9 | |
| Asthma | 424 | 3.1 | 2.9-3.2 | |
| Allergy | 492 | 3 | 2.8-3.1 | |
| VAS Nasal Discharge | Overall | 1549 | 54.3 | 50.5-58.2 |
| CRSwNP | 318 | 57.2** | 44.4-69.9 | |
| CRSsNP | 133 | 45.5 | 45.4-45.6 | |
| Asthma | 107 | 61.2 | 50-72.3 | |
| Allergy | - | - | - | |
| VAS Postnasal Discharge | Overall | 1550 | 57.2 | 54.2-60.1 |
| CRSwNP | 446 | 57.6** | 50-65.1 | |
| CRSsNP | 147 | 46.6 | 22.2-70.9 | |
| Asthma | 75 | 68 | 42.2-93.8 | |
| Allergy | 14 | 79.3 | 68.5-90.1 | |
| VAS Rhinorrhoea | Overall | 1892 | 57.3 | 51.7-62.9 |
| CRSwNP | 1415 | 64.5** | 61.9-67.1 | |
| CRSsNP | 73 | 48.9 | 24.9-72.9 | |
| Asthma | 56 | 74.6 | 60.6-88.6 | |
| Allergy | 14 | 60.7 | 46.3-71.1 | |
| CI, confidence interval; CRSwNP, chronic rhinosinusitis with nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps Total SNOT22: 0-110 scale; Individual SNOT22 symptom: 0-5 scale; VAS: 0-100 scale *Greater than CRSwNP group (p < 0.05) **Greater than CRSsNP group (p < 0.05) ***Greater than both CRSwNP and CRSsNP groups (p < 0.05) | ||||
References
- Orlandi R, Kingdom T, Smith T. International consensus statement on allergy and rhinology: rhinosinusitis 2021. Int Forum Allergy Rhinol. 2021;11:213-739. doi:https://doi.org/10.1002/alr.22741
- Hopkins C, Gillett S, Slack R. Psychometric validity of the 22-item sinonasal outcome test. Clin Otolaryngol. 2009;34:447-454. doi:https://doi.org/10.1111/j.1749-4486.2009.01995.x
- Browne J, Hopkins C, Slack R. The Sino-Nasal Outcome Test (SNOT): can we make it more clinically meaningful?. Otolaryngol Head Neck Surg. 2007;136:736-741. doi:https://doi.org/10.1016/j.otohns.2007.01.024
- Mattos J, Rudmik L, Schlosser R. Symptom importance, patient expectations, and satisfaction in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2019;9:593-600. doi:https://doi.org/10.1002/alr.22309
- McCoul E, Mohammed A, Debbaneh P. Differences in the intended meaning of congestion between patients and clinicians. JAMA Otolaryngol Head Neck Surg. 2019;145:634-640. doi:https://doi.org/10.1001/jamaoto.2019.1023
- Fischer J, Tolisano A, Navarro A. Are you congested? A comparison of definitions between otolaryngologists and their patients. Int Forum Allergy Rhinol. 2024;14:86-95. doi:https://doi.org/10.1002/alr.23228
- Bohnhorst I, Jawad S, Lange B. Prevalence of chronic rhinosinusitis in a population of patients with gastroesophageal reflux disease. Am J Rhinol Allergy. 2015;29:E70-E74. doi:https://doi.org/10.2500/ajra.2015.29.4167
- Schlosser R, Smith T, Mace J. Asthma quality of life and control after sinus surgery in patients with chronic rhinosinusitis. Allergy. 2017;72:483-491. doi:https://doi.org/10.1111/all.13048
- Heiland L, Farmer H, Nguyen S. Headache and facial pain/pressure in the chronic rhinosinusitis population: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2024;171:1308-1320. doi:https://doi.org/10.1002/ohn.855
- Page M, McKenzie J, Bossuyt P. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372. doi:https://doi.org/10.1136/bmj.n71
- The Oxford Levels of Evidence 2. Oxford Centre for Evidence Based Medicine. Published online 2011.
- Sterne J, Hernán M, Reeves B. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj. 2016;355. doi:https://doi.org/10.1136/bmj.i4919
- Sterne J, Savović J, Page M. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366. doi:https://doi.org/10.1136/bmj.l4898
- Munn Z, Barker T, Moola S. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18:2127-2133. doi:https://doi.org/10.11124/jbisrir-d-19-00099
- Higgins J, Thomas J, Chandler J. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.4. Cochrane; 2023.
- McGrath S, Sohn H, Steele R. Meta-analysis of the difference of medians. Biom J. 2020;62:69-98. doi:https://doi.org/10.1002/bimj.201900036
- McGrath S, Zhao X, Qin Z. One-sample aggregate data meta-analysis of medians. Stat Med. 2019;38:969-984. doi:https://doi.org/10.1002/sim.8013
- Sterne J, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046-1055. doi:https://doi.org/10.1016/s0895-4356(01)00377-8
- Egger M, Davey Smith G, Schneider M. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629-634. doi:https://doi.org/10.1136/bmj.315.7109.629
- Zeng M, Long X-B, Cui Y-H. Comparison of efficacy of mometasone furoate versus clarithromycin in the treatment of chronic rhinosinusitis without nasal polyps in Chinese adults. Am J Rhinol Allergy. 2011;25:E203-E207. doi:https://doi.org/10.2500/ajra.2011.25.3728
- Yu L, Jiang Y, Yan B. Predictive value of clinical characteristics in eosinophilic chronic rhinosinusitis with nasal polyps: a cross-sectional study in the Chinese population. Int Forum Allergy Rhinol. 2022;12:726-734. doi:https://doi.org/10.1002/alr.22901
- Young J, Frenkiel S, Tewfik M. Long-term outcome analysis of endoscopic sinus surgery for chronic sinusitis. Am J Rhinol. 2007;21:743-747. doi:https://doi.org/10.2500/ajr.2007.21.3108
- Xu Q, Du K, Zheng M. Application of clinical scores in the differential diagnosis of chronic rhinosinusitis with nasal polyps in a Chinese population. Am J Rhinol Allergy. 2020;34:401-408. doi:https://doi.org/10.1177/1945892420901996
- Verma P, Rawat D, Aseri Y. A prospective longitudinal study of clinical outcome and quality of life assessment in patients with chronic rhinosinusitis after functional endoscopic sinus surgery using sino nasal outcome test-22. Ind J Otolaryngol Head Neck Surg. 2022;74:792-799. doi:https://doi.org/10.1007/s12070-020-01847-4
- Tomljenovic D, Pinter D, Kalogjera L. Perceived stress and severity of chronic rhinosinusitis in allergic and nonallergic patients. Allergy Asthma Proc. 2014;35:398-403. doi:https://doi.org/10.2500/aap.2014.35.3774
- Tiotiu A, Oster J, Roux P. Effectiveness of omalizumab in severe allergic asthma and nasal polyposis: a real-life study. J Investig Allergol Clin Immunol. 2020;30:49-57. doi:https://doi.org/10.18176/jiaci.0391
- Thunberg U, Saber A, Söderquist B. Long-term clinical follow-up of patients with chronic rhinosinusitis. Ann Otol Rhinol Laryngol. 2021;130:504-512. doi:https://doi.org/10.1177/0003489420962822
- Tat T. Omalizumab is effective in nasal polyposis with or without asthma, a real-life study. World Allergy Organ J. 2022;15. doi:https://doi.org/10.1016/j.waojou.2022.100670
- Suh J, Wu A, Taw M. Treatment of recalcitrant chronic rhinosinusitis with integrative east-west medicine: a pilot study. Arch Otolaryngol Head Neck Surg. 2012;138:294-300. doi:https://doi.org/10.1001/archoto.2011.1489
- Stolovitzky J, Kern R, Han J. In-office placement of mometasone furoate sinus implants for recurrent nasal polyps: a pooled analysis. Am J Rhinol Allergy. 2019;33:545-558. doi:https://doi.org/10.1177/1945892419850924
- Soler Z, Mace J, Smith T. Symptom-based presentation of chronic rhinosinusitis and symptom-specific outcomes after endoscopic sinus surgery. Am J Rhinol. 2008;22:297-301. doi:https://doi.org/10.2500/ajr.2008.22.3172
- Sima Y, Zhang J, Zheng M. Revision surgery versus biologic treatment with omalizumab in recurrent chronic rhinosinusitis with nasal polyps: an analysis of cost-utility and clinical outcomes. World Allergy Organ J. 2023;16. doi:https://doi.org/10.1016/j.waojou.2023.100846
- Shao S, Wang Y, Zhang N. A prospective single-arm study on the efficacy and safety of short-course oral corticosteroids followed by topical corticosteroids in patients with severe chronic rhinosinusitis with nasal polyps. Expert Rev Clin Immunol. 2023;19:1029-1039. doi:https://doi.org/10.1080/1744666x.2023.2209724
- Savietto E, Marioni G, Maculan P. Effectiveness of micronized nasal irrigations with hyaluronic acid/isotonic saline solution in non-polipoid chronic rhinosinusitis: a prospective, randomized, double-blind, controlled study. Am J Otolaryngol. 2020;41. doi:https://doi.org/10.1016/j.amjoto.2020.102502
- Qi Y, Liu J, Peng S. Efficacy of selective vidian neurectomy for allergic rhinitis combined with chronic rhinosinusitis. ORL J Otorhinolaryngol Relat Spec. 2021;83:327-334. doi:https://doi.org/10.1159/000512083
- Pham H, Nguyen T, Tran T. A comparison of effectiveness between Posisep and Merocel nasal packing after endoscopic sinus surgery: findings from a randomized, double-blinded, controlled trial. Randomized Controlled Trial Medicine. 2023;102(32). doi:https://doi.org/10.1097/MD.0000000000034782
- Penezić A, Paić M, Gregurić T. The impact of asthma on quality of life and symptoms in patients with chronic rhinosinusitis. Curr Med Res Opin. 2020;36:1043-1048. doi:https://doi.org/10.1080/03007995.2020.1754189
- Paoletti G, Casini M, Malvezzi L. Very rapid improvement in extended nitric oxide parameters is associated with clinical and functional improvement in patients with chronic rhinosinusitis with nasal polyps treated with dupilumab. J Investig Allergol Clin Immunol. 2023;33:457-463. doi:https://doi.org/10.18176/jiaci.0851
- Pan X, Zhang Y, Wang C. Evaluation of nasal symptoms to distinguish eosinophilic from noneosinophilic nasal polyps based on peripheral blood. Allergy Asthma Proc. 2021;42:214-221. doi:https://doi.org/10.2500/aap.2021.42.210004
- Paçacı Çetin G, Arslan B, Yılmaz İ. Doxycycline may be more clinically effective in type 2 chronic rhinosinusitis nasal polyp comorbid with asthma. J Asthma. 2024;61:20-26. doi:https://doi.org/10.1080/02770903.2023.2236696
- Niknami M, Emami E, Mozaffari A. Correlation between the opacification degree of paranasal sinuses on CT, clinical symptoms and anatomical variations of the nose and paranasal sinuses in patients with chronic rhinosinusitis. Front Dent. 2021;18. doi:https://doi.org/10.18502/fid.v18i33.7337
- Nguyen D, Arous F, Gallet P. Sinonasal symptom-related sleep disorders before and after surgery for nasal polyposis. Rhinology. 2017;55:262-268. doi:https://doi.org/10.4193/Rhin16.016
- Nabavi M, Arshi S, Bemanian M. Doxycycline improves quality of life and anosmia in chronic rhinosinusitis with nasal polyposis: a randomized controlled trial. Am J Rhinol Allergy. 2023;37:384-390. doi:https://doi.org/10.1177/19458924231154066
- Lourijsen E, Reitsma S, Vleming M. Endoscopic sinus surgery with medical therapy versus medical therapy for chronic rhinosinusitis with nasal polyps: a multicentre, randomised, controlled trial. Lancet Respir Med. 2022;10:337-346. doi:https://doi.org/10.1016/S2213-2600(21)00457-4
- Liu M, Woodworth B, Kanaan A. SNOT-22 quality of life scores improve after endoscopic endonasal repair of spontaneous cerebrospinal fluid rhinorrhea. Ann Otol Rhinol Laryngol. 2023;132:1077-1084. doi:https://doi.org/10.1177/00034894221133769
- Liu M, Gardner J, Woodworth B. Individual SNOT-22 items aid in differentiating between spontaneous cerebrospinal fluid rhinorrhea and chronic rhinosinusitis without nasal polyps. Ann Otol Rhinol Laryngol. 2023;132:698-704. doi:https://doi.org/10.1177/00034894221111256
- Liu C, Han E, Fischer J. Patient perspectives on chronic rhinosinusitis in cystic fibrosis: symptom prioritization in the era of highly effective modulator therapy. Int Forum Allergy Rhinol. 2024;14:1282-1293. doi:https://doi.org/10.1002/alr.23332
- Ling F, Kountakis S. Important clinical symptoms in patients undergoing functional endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2007;117:1090-1093. doi:https://doi.org/10.1097/mlg.0b013e31804b1a90
- Ling F, Kountakis S. Rhinosinusitis task force symptoms versus the sinonasal outcomes test in patients evaluated for chronic rhinosinusitis. Am J Rhinol. 2007;21:495-498. doi:https://doi.org/10.2500/ajr.2007.21.3052
- Lal D, Rounds A, Divekar R. Gender-specific differences in chronic rhinosinusitis patients electing endoscopic sinus surgery. Int Forum Allergy Rhinol. 2016;6:278-286. doi:https://doi.org/10.1002/alr.21667
- Ji K, Risoli T, Kuchibhatla M. Symptom profile of chronic rhinosinusitis versus obstructive sleep apnea in a tertiary rhinology clinic. Ann Otol Rhinol Laryngol. 2019;128:963-969. doi:https://doi.org/10.1177/0003489419851527
- Jamtøy K, Tronvik E, Bratbak D. OnabotulinumtoxinA injection towards the SPG for treating symptoms of refractory chronic rhinosinusitis with nasal polyposis: a pilot study. Acta Otolaryngol. 2021;141:934-940. doi:https://doi.org/10.1080/00016489.2021.1982146
- Huang Z-Z, Chen X-Z, Huang J-C. Budesonide nasal irrigation improved Lund–Kennedy endoscopic score of chronic rhinosinusitis patients after endoscopic sinus surgery. Eur Arch Otorhinolaryngol. 2019;276:1397-1403. doi:https://doi.org/10.1007/s00405-019-05327-6
- Hao D, Wu Y, Li P. An integrated analysis of inflammatory endotypes and clinical characteristics in chronic rhinosinusitis with nasal polyps. J Inflam Res. 2022;15:5557-5565. doi:https://doi.org/10.2147/jir.s377301
- Guo Y, Nie Z, Chen C. Outcomes of endoscopic sinus surgery in patients with central compartment atopic disease. World Allergy Organ J. 2024;17. doi:https://doi.org/10.1016/j.waojou.2023.100859
- Gregurić T, Baudoin T, Tomljenović D. Relationship between nasal septal deformity, symptoms and disease severity in chronic rhinosinusitis. Eur Arch Otorhinolaryngol. 2016;273:671-677. doi:https://doi.org/10.1007/s00405-015-3615-8
- Gelardi M, Bocciolini C, Notargiacomo M. Chronic rhinosinusitis with nasal polyps: how to identify eligible patients for biologics in clinical practice. Acta Otorhinolaryngol Ital. 2022;42:75-81. doi:https://doi.org/10.14639/0392-100x-n1699
- Ebbens F, Scadding G, Badia L. Amphotericin B nasal lavages: not a solution for patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2006;118:1149-1156. doi:https://doi.org/10.1016/j.jaci.2006.07.058
- De Corso E, Porru D, Corbò M. Comparative real-world outcomes of dupilumab versus endoscopic sinus surgery in the treatment of severe CRSwNP patients. Clin Otolaryngol. 2024;49:481-489. doi:https://doi.org/10.1111/coa.14172
- Dabirmoghaddam P, Mehdizadeh Seraj J, Bastaninejad S. The efficacy of clarithromycin in patients with severe nasal polyposis. Acta Med Iran. 2013;51:359-364.
- De Corso E, Pasquini E, Trimarchi M. Dupilumab in the treatment of severe uncontrolled chronic rhinosinusitis with nasal polyps (CRSwNP): a multicentric observational Phase IV real-life study (DUPIREAL). Allergy. 2023;78:2669-2683. doi:https://doi.org/10.1111/all.15772
- Chen F-H, Deng J, Hong H-Y. Extensive versus functional endoscopic sinus surgery for chronic rhinosinusitis with nasal polyps and asthma: a 1-year study. Am J Rhinol Allergy. 2016;30:143-148. doi:https://doi.org/10.2500/ajra.2016.30.4271
- Cervin A, Kalm O, Sandkull P. One-year low-dose erythromycin treatment of persistent chronic sinusitis after sinus surgery: clinical outcome and effects on mucociliary parameters and nasal nitric oxide. Otolaryngol Head Neck Surg. 2002;126:481-489. doi:https://doi.org/10.1067/mhn.2002.124849
- Byun J, Lee J. Canine fossa puncture for severe maxillary disease in unilateral chronic sinusitis with nasal polyp. Laryngoscope. 2013;123:E79-E84. doi:https://doi.org/10.1002/lary.24274
- Bachert C, Sousa A, Lund V. Reduced need for surgery in severe nasal polyposis with mepolizumab: randomized trial. J Allergy Clin Immunol. 2017;140:1024-1031.e14. doi:https://doi.org/10.1016/j.jaci.2017.05.044
- Alicandri-Ciufelli M, Marchioni D, Pipolo C. Influence of prior endoscopic sinus surgery extent on dupilumab effectiveness in CRSwNP patients. Laryngoscope. 2024;134:1556-1563. doi:https://doi.org/10.1002/lary.30983
- Zhou H, Zhang W, Gong W. [Efficacy of glucocorticoid stent implantation in ethmoid sinus after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyps]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2023;37:252-257. doi:https://doi.org/10.13201/j.issn.2096-7993.2023.04.003
- Ghadersohi S, Price C, Beaumont J. Responsiveness and convergent validity of a new patient-reported outcome measure for chronic rhinosinusitis (CRS-PRO). J Allergy Clin Immunol Pract. 2020;8:2351-2359.e2. doi:https://doi.org/10.1016/j.jaip.2020.04.031
- Piccirillo J, Merritt M, Richards M. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002;126:41-47. doi:https://doi.org/10.1067/mhn.2002.121022
- Stevens W, Peters A, Tan B. Associations between inflammatory endotypes and clinical presentations in chronic rhinosinusitis. J Allergy Clin Immunol Pract. 2019;7:2812-2820.e3. doi:https://doi.org/10.1016/j.jaip.2019.05.009
- Huang C, Chang P, Wu P. Impact of nasal symptoms on the evaluation of asthma control. Medicine. 2017;96. doi:https://doi.org/10.1097/md.0000000000006147
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 986 times
- PDF downloaded - 224 times



