Reviews
Vol. 45: Issue 2 - April 2025
The impact of immunonutrition in head and neck cancer surgery: a systematic review with meta-analysis
Abstract
Objective. Malnutrition is common among patients undergoing surgery for head and neck cancer (HNC), leading to higher postoperative complications and mortality rates. Immunonutritional intervention has potential in reducing these risks by enhancing immune function and aiding wound healing.
Methods. A systematic review and meta-analysis were conducted according to PRISMA guidelines. Nineteen randomised controlled trials involving 1,196 participants undergoing surgery for HNC were included. Studies comparing immunonutrition with standard care were analysed for outcomes including fistula formation, wound infections, other infections, and length of hospital stay.
Results. Immunonutrition significantly reduced postoperative fistulas and shortened hospital stays compared to standard care. The impact on wound and systemic infections was inconclusive. Immunonutrition was generally well-tolerated, with no significant increase in adverse events.
Conclusions. These findings highlight the potential benefits of immunonutrition in improving postoperative outcomes for patients with HNC. However, the variability in study outcomes and limitations in quality call for further research to clarify the specific efficacy, long-term effects, and cost-effectiveness of immunonutrition in this context.
Introduction
Malnutrition is prevalent in more than 50% of patients with head and neck cancer (HNC) 1 and results from various factors, including difficulties in eating, inflammatory response triggered by tumours, poor dietary habits, and adverse effects of surgical procedures, chemotherapy, and radiotherapy 2. Malnourished patients have well-documented immune deficits which, combined with the immune-suppressive effect of surgery, may lead to increased postoperative complications, including impaired wound healing, local and systemic infection, cardiac and respiratory dysfunction, increased length of hospital stay and mortality 1,3. Major surgery for HNC often requires mucosal incision in contaminated areas such as the oral cavity, nose and paranasal sinuses, oropharynx, larynx, hypopharynx, or cervical oesophagus. These regions typically harbour microorganisms found on mucous surfaces 4. This type of wound, considered “clean-contaminated,” carries a significant risk, potentially as high as 50%, for surgical complications, which include the development of cutaneous fistulas and wound infections 4-6. A cutaneous fistula, which can manifest as oro-or pharyngo-cutaneous, stands as one of the most severe complications and can result in significant health issues encompassing carotid artery/jugular vein blowout, mediastinitis, aspiration pneumonia, sepsis, and, in some cases, even death. Furthermore, these postoperative problems usually prolong hospitalisation, possibly causing a delay in adjuvant therapies, which in turn may lead to a decreased efficacy of the overall treatment strategy. In addition, they may greatly impact the patient’s quality of life due to delays in resuming oral intake and voice rehabilitation.
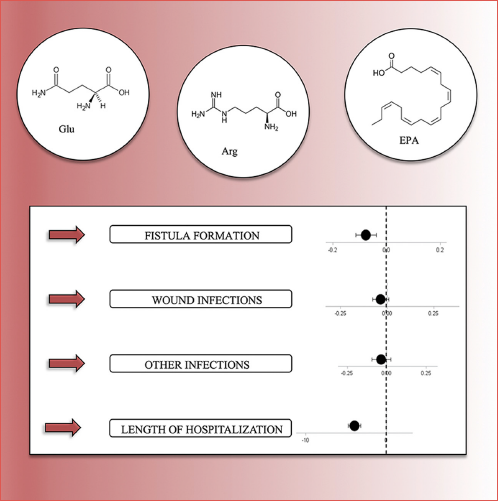
It is now established that certain substances, in addition to their primary role in providing essential nutrients, are associated with pharmacological-like effects on the immunity system. These immune-boosting nutrients encompass a wide range of compounds, including fats like n-3 fatty acids, amino acids such as arginine and glutamine, and vitamins like vitamin E, as well as other elements like nucleotides and antioxidants. These can be administered either through the digestive system or intravenously. Existing evidence suggests that nutritional supplements containing these immune-enhancing additives can positively influence the immune and inflammatory responses, both in laboratory settings and in patients dealing with trauma, burns, or gastrointestinal surgery 7-9. Meta-analyses indicate that immunonutrition can reduce the occurrence of infectious complications in critically-ill patients 10 and in patients with HNC 11,12. Moreover, particular attention to immunonutrition has been given in the last years, especially with the implementation of the Enhanced Recovery After Surgery (ERAS) programmes, adding complexity to the assessment of this particular treatment 13-15. A standard nutritional diet contains whole protein, partially digested starch and triglycerides, electrolytes, trace elements, and vitamins. The most extensively studied nutrients in immunonutrition formulas are arginine, glutamine, omega-3 fatty acids, and nucleotides. Arginine, the most commonly used immunonutrient for patients with HNC, is a non-essential amino acid with roles in nucleotide synthesis, polyamine production, nitric oxide generation, and proline formation. Arginine can potentially enhance lymphocytic function and facilitate wound healing. Glutamine, another amino acid, serves as an energy source for rapidly dividing cells in the body, especially enterocytes and colonocytes. The addition of omega-3 fatty acids to enteral nutrition feeds can reduce proinflammatory factors in stressed patients and with the potential to lower the rates of infection. The specific content of immunonutrition formulas may vary among products.
The present systematic review and meta-analysis is aimed at evaluating the current evidence on the impact of enriched nutritional formulas on surgical outcomes in patients with HNC.
Materials and methods
The systematic review and meta-analysis adhered to the principles outlined in the PRISMA declaration 16.
Inclusion criteria
Studies were eligible for inclusion if: 1) were randomised, double-blinded, controlled trials; 2) included as target population patients undergoing surgery for HNC; 3) compared standard care vs. immunoenhanced nutritional formulas in pre- and/or postoperative settings; 4) enrolled adults aged 18 years or older; 5) were written in English.
Exclusion criteria
The exclusion criteria encompassed non-randomised studies and treatment strategies not including surgery.
Intervention
The intervention involved the administration of polymeric nutritional supplements enriched with immunonutritional additives through either oral or enteral routes. Studies eligible for inclusion were required to administer immunonutrition either before and/or after the surgical procedure. Co-administration of other oral or parenteral substances was allowed, provided that the quantity of immunonutritional additives was quantified. It is worth noting that the composition of immunonutrition formulas can vary across different products, and we documented the specific product used in each study.
Control
The control group received standard care, which typically included intravenous fluids and/or polymeric nutritional supplements. The comparison was between immunonutrition and standard care.
Outcomes
The primary outcome of interest was to evaluate the impact of immune-enhanced nutritional formulas on the occurrence of postoperative complications, such as fistulas, surgical site infections, and other infections. Additionally, the review aimed to assess the effect of these formulas on the in-hospital length of stay (LoS). Secondary outcomes included mortality and adverse effects associated with enteral nutrition, such as diarrhoea.
Search methods for identification of studies
A comprehensive bibliographic search was performed across multiple databases, including PubMed, Embase, and the Cochrane Library. The search terms employed included “Head and neck neoplasms”, “Head and neck cancer”, “Nutritional intervention”, “Immunonutrition”, “Prehabilitation”, and “Complication rate”. These terms were combined using the Boolean operators “AND” and “OR”.
Selection of studies
Two review authors (CLM, GT) independently examined the titles and abstracts of studies identified through the search strategy. Inconsistency between review authors regarding articles for full-text reading was resolved by consultation with senior authors. We obtained full-text papers for all studies that could not be excluded on the basis of title and abstract. The same review authors then independently refined their selection by examining the articles selected and excluding those not relevant to the review. The review authors recorded agreement on study inclusion and resolved disagreement by consensus. We documented decisions on all studies and these are presented in the PRISMA flow-chart (Fig. 1).
The randomised controlled trials identified were considered suitable for review if they met the initial inclusion criteria.
Statistical analysis
Quantitative data, including mean and standard deviation for each variable, as well as frequency of measured qualitative outcomes, were extracted. A meta-analysis was performed calculating proportions and mean differences (MD) along with 95% confidence intervals (95% CI). Heterogeneity, representing differences among studies that may affect result aggregation, was assessed using the Q test, with heterogeneity considered present when p < 0.05. Significant differences between interventions were considered when the 95% CI did not include the value 0 (for MD).
Results
The electronic searches retrieved 1,765 results. We identified 3 further records through scanning the reference lists of studies. After selecting 90 articles by title, we screened titles and abstracts, finding 28 records. We sought full texts for all of the selected reports and excluded a further 8 records because they were not matching inclusion criteria. Finally, 19 studies were included in the systematic review and 16 were selected for quantitative comparison in the meta-analysis. The characteristics of the studies included are in Table I.
Setting
Studies were set in hospitals and conducted in 9 countries: 8 from Spain 1,17-19, 2 from the USA 20,21, 2 from Thailand 22,23, and one each from Greece 24, France 25, Italy 26, Netherlands 27, New Zealand 28, Japan 29, and UK 30. Eighteen studies were single-site studies and one was multicentre 25.
Participants
The 19 studies included encompassed 1,196 participants undergoing surgery of the upper aerodigestive tract (sites included oral cavity, pharynx, and larynx) for HNC (Tab. II).
Studies included adults only and the mean age of study participants ranged from 47 to 66 years. There were more males than females in most studies, and the mean body mass index (BMI) ranged from 19.9 to 26.5 kg/m2. Studies excluded people with a range of medical conditions including impaired renal or hepatic function, ongoing infections and autoimmune disorders, those on steroid treatment or nutritional oral supplementation in the previous 6 months and those who were malnourished/had severe cancer cachexia or sarcopenia, those who were morbidly obese, patients with contraindications to enteral nutrition/patients with inborn errors of metabolism relating to the composition of the formula, patients treated with chemotherapy and/or radiation therapy delivered to the head and neck during the previous year or chemoradiotherapy or other treatment protocols concurrent to the intervention, patients testing positive for HIV, patients with diabetes, and pregnant or breast-feeding women. In all the studies reported, patients were randomly assigned to one of two treatment groups according to a computer-generated 1:1 randomisation schedule.
Intervention
The intervention group consisted of 620 patients. The various approaches employed in the studies are listed in Table I. The majority (14 of 19) used immunonutrition formulas containing arginine, 2 studies employed glutamine powder, 2 others used an eicosapentaenoic acid (EPA)-enriched oral nutritional supplement, and one employed an unspecified product. In cases where the intervention was administered preoperatively, the duration ranged from approximately 5 to 14 days (in 10 studies). In contrast, when feeds were given postoperatively, there was more variability, with durations ranging from approximately 5 days to an average of 22 days ± 12 (in 18 studies).
The control group of 576 patients received, in most studies (17 of 19), a commercial polymeric feed postoperatively, some of which contained additional fibre. In 5 studies, the control group received a standard polymeric feed both pre- and postoperatively 21,24,25,27,30. Additionally, in one study, 2 groups were combined in the analyses, with one group having received the control feed both pre- and postoperatively, and the other only receiving it postoperatively 20. The follow-up times for survival data differed significantly among studies, ranging from 5 postoperative days 31 to more than 16 months 27.
Primary outcomes
FISTULA FORMATION
Fistula was reported in 12 studies. The absolute risk ranged between 0% 21,24,32 to 13% 22 in the immunonutrition groups, and between 2% 20 to 29% 21 in the control groups. The events were almost halved passing from the control group (a total of 58 events among 441 patients, or 13%) to the immunoenhanced group (a total of 27 events among 484 patients, or 6%). Only in one study 20 were fistulas more represented in the intervention group than in the control group. The meta-analysis showed a statistically significant reduction in fistula formation with immunonutrition compared to standard care: the combined difference was -0.077 (95% CI -0.115 to -0.039, 12 studies, n = 925) (Fig. 2).
WOUND INFECTIONS
Wound infections were reported in 12 studies including 855 patients. In one study ‘wound complications’ was reported 24. The Additional treatment, Serous discharge, Erythema, Purulent exudate, Separation of deep tissues, Isolation of bacteria, and Stay as inpatient prolonged over 14 days (ASEPSIS) scoring method 33 was mainly used to assess the presence of surgical site infections. In 2 studies 25,28 infectious complications were judged using CDC criteria and were considered significant if antibiotic therapy was instituted. Absolute risks ranged from 3% 19 to 61% 30 in the immunonutrition groups, and from 0% 21,28 to 59% 30 in the control groups. Events were slightly more common in the control group (79 events among 406 participants, 19%) than in the immunoenhanced group (68 events among 449 participants, 15%). A meta-analysis of the results of these studies found no significant reduction in the risk of postoperative wound infection with a difference between proportions of -0.035 (95% CI of -0.078 to 0.009, 13 studies, n = 855) (Fig. 3).
EFFECTS ON OTHER INFECTIONS
The presence of infections in locations other than the surgical site (e.g. respiratory tract infection diagnosed with chest X-rays, temperature above 38.5°C, and isolation of pathogens from the sputum and/or blood culture and/or urinary tract infection) was evaluated in 10 trials including 682 patients, 360 receiving immunonutrition and 154 receiving standard care. The prevalence of infections ranged between 0% 1,28 to 43% 30 with immunonutrition, and between 0% 22 to 50% 28 with an isonitrogenous-isocaloric diet. When all the trials that reported this outcome were included in the meta-analysis, there was no statistically significant difference between interventions: the combined difference was -0.034 (95% CI -0.094 to 0.027, 10 studies, n = 628) (Fig. 4).
IN-HOSPITAL LENGTH OF STAY
LoS was reported in 12 studies and was defined as the time from surgery to the date when the patient was deemed medically fit for discharge in all studies. The mean LoS ranged from 15.3 to 31.1 days in the immunonutrition groups and from 17.4 to 46.1 days in the control group. We found evidence of a statistically significant reduction of LoS when nutritional support was given through immunoenhanced formulas with a difference of -3.937 (95% CI -4.699 to -3.174, 12 studies, n = 905) (Fig. 5).
SECONDARY OUTCOMES
Many of the studies also analysed the influence of immunoenhanced nutrition on inflammatory response, gastrointestinal problems related to enteral feeding, and survival. These parameters were not included in the present meta-analysis, but were included in the review.
INFLAMMATORY RESPONSE
This outcome was assessed by measuring serum levels of albumin, prealbumin, transferrin, total number of lymphocytes, lymphocyte subsets, and serum immunoglobulin concentrations, along with interleukin-6, tumour necrosis factor-α, and C-reactive protein levels both before and after surgery. Upon analysing the reported outcomes, it became apparent that, particularly in malnourished patients, the addition of immunomodulatory agents may lead to an upregulation of immune function, which could be associated with reduced recovery time and improved wound healing. However, no study reported a significant relationship between serum levels of inflammatory markers and postoperative recovery 1,17-19,21,24-26,29,31,32,34,35.
GASTROINTESTINAL TOLERANCE
Gastrointestinal problems related to enteral feeding were recorded in 6 studies 1,17,19,20,32,35 as the presence of diarrhoea (> 5 liquid stools in a 24 h period or an estimated volume > 2000 ml/day) compared in the 2 groups. Immunoenhanced formulas were as well tolerated as the standard ones.
SURVIVAL
Only 5 studies reported survival information 24,25,27,30,32. The follow-up periods varied significantly, ranging from the time until hospital discharge to 3 months, and not all of the studies reported the cause and timing of patient deaths. However, all the studies concurred that there was no significant difference in survival between the 2 groups, although there was a trend toward better survival for patients in the immunoenhanced supplement group.
Discussion
This systematic review and meta-analysis, involving 19 studies, aimed at investigating the impact of immune-enhanced formulas on clinical outcomes in patients undergoing surgery for HNC. The main objective was to assess the principal benefits of immune-enhanced formulas for surgical patients, who are often malnourished and at a higher risk of complications. This meta-analysis focused exclusively on the impact of nutritional intervention on clinical outcomes, prioritising these over other parameters like inflammation or immune response. The combined results indicated a reduction in the LoS in the groups receiving immunonutrition, along with a decrease in the risk of fistula formation. On the other hand, immunonutrition appeared to have little to no effect on wound infections and systemic infections, which, according to the meta-analysis, were overall reduced in the intervention group, but without statistical significance. Adverse events like diarrhoea showed little or no difference between the treatment groups, and therefore immunonutrition seems generally well tolerated. Other complications were not formally analysed due to their heterogeneity. The timing of intervention (pre- and postoperative, or only postoperative) did not substantially impact the results, except for one study that reported more fistulas with immunonutrition when administered both before and after surgery 20. At the same time, some authors 19,22,30 reported more general infections in the immunonutrition group. These findings are inconsistent with other studies, regardless of the timing of intervention, which showed fewer fistulas and complications with immunonutrition compared to standard care. The reasons for these discrepancies remain unclear. Mortality was often inadequately reported, making it inappropriate to attribute any difference in mortality to immunonutrition. Nevertheless, there was no evidence of any effect of immunonutrition on mortality.
This systematic review can be considered as an update to the systematic review of Howes et al. 11. From its publication in 2018, 2 more randomised controlled trials on the subject were published which matched the inclusion criteria. With our update, we were able to confirm the potential positive effect of immunonutrition in reducing fistula formation after HNC surgery, but we also found that there may also be a stronger impact on LoS reduction with this kind of nutritional intervention.
The relatively recent introduction of ERAS programmes in some healthcare systems complicates the evaluation of specific interventions such as immunonutrition. ERAS programmes encompass multiple potentially effective interventions throughout the perioperative period, including minimally invasive surgical techniques, effective pain management, early postoperative feeding, and mobilisation 13. A recent review of the ERAS protocol implementation demonstrated the importance of these perioperative actions in reducing LoS and opioid use in patients undergoing surgery for HNC, with or without microvascular reconstruction 36. Future studies need to address the challenge of discerning the contribution of individual interventions, as in this case immunonutrition, compared to standard care, in order to assess which intervention are the most effective in order to improve recovery and quality of life, and possibly simplify the treatment protocol.
Another area that warrants study is the role of immunonutrition before major HNC surgery in the elderly, especially when frail and malnourished, since this subset of the population is becoming increasingly more represented in the daily surgical activity of referral, tertiary, large volume HNC centres 37,38. On the other hand, people > 65 years tend to be underrepresented in most prospective clinical trials, without exception for those related to the described immunonutrition protocols 1,23,25,30. Addressing this research gap could provide critical insights and improve clinical care strategies for this growing demographic group.
The main limitation of this systematic review is represented by the small number of high-quality studies found. Both blinding and randomisation methods were not always fully reported in most trials. On the other hand, all studies had small sample sizes, and the results of the analysis were not always shown exhaustively. In addition, there was no homogeneity in the outcomes assessed or in their definition. In general, most studies were underpowered to provide precise estimates of the effects of the intervention.
According to the present data, further randomised, controlled trials of higher methodological quality are needed. These studies require a sufficient sample size to study low frequency outcomes such as infections and death. This meta-analysis shows the beneficial effects of perioperative immunonutrition in HNC surgery patients, but with weak evidence. As most of the studies selected in this review included a specific mixture of nutrients, more research is needed to assess the specific efficacy of each of them. Likewise, the best schedule (pre- and/or postoperative) and duration of administration is to be clarified. There is currently some evidence that perioperative immunonutrition is cost-effective in gastrointestinal surgery, despite the higher costs of these formulas. However, although a significant reduction in resource consumption is implied by the shortening of LoS, specific studies are needed to establish the cost-effectiveness of immunonutrition in HNC. Finally, data about the long-term effects of immunonutrition in HNC patients, which theoretically may include prolonged survival, reduced treatment-related toxicity, and better quality of life, are scarce.
Conclusions
This systematic review and meta-analysis suggest that the administration of immunoenriched nutrition in HNC patients undergoing surgery may reduce the occurrence of postoperative fistulas and LoS. These results seem to be related to the perioperative administration of these formulas and seem to reinforce the ERAS guidelines on enteral nutrition. More trials with better methodological quality and larger sample sizes are needed to assess the effects of perioperative immunonutrition, long-term outcomes, and the cost-effectiveness of this nutritional intervention.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
CLM, GT, DM: study design, article selection, review drafting and critical revision; CLM, GT: article search and selection, data extraction; LT: pooled analysis and critical revision; DM, CP: critical revision of the article.
Ethical consideration
No formal ethics committee approval was required for this article as it is based on already published clinical data from other studies available in the literature.
History
Received: July 5, 2024
Accepted: August 26, 2024
Figures and tables
Figure 1. PRISMA flow-chart of screening process.
Figure 2. Forest plot evaluating the impact of immunoenhanced nutrition vs standard care on fistula formation.
Figure 3. Forest plot evaluating the impact of immunoenhanced nutrition vs standard care on wound infections.
Figure 4. Forest plot evaluating the impact of immunoenhanced nutrition vs standard care on other infections.
Figure 5. Forest plot evaluating the impact of immunoenhanced nutrition vs standard care on LoS.
| Article | Year | Study characteristics | Intervention | Follow-up(days) | ||||
|---|---|---|---|---|---|---|---|---|
| Design | N (I – C) | Pre (days) | Post (days) | Control | Immunoenhanced formula | |||
| Snyderman 20 | 1999 | RCT | 129 (82-47) | ≥ 5 | ≥ 7 | Standard formula | Arginine, RNA and omega-3 fatty acids (Impact, Nestle) | 30d |
| Riso 26 | 2000 | RCT | 44 (23-21) | / | ≥ 10 (following total laryngectomy) or ≥ 21 (following partial laryngectomy) | Standard formula | Arginine-enhanced formula | Until hospital discharge |
| Van Bokhorst 27 | 2000 | RCT | 32 (17-15) | 7-10 | ≥ 10 | Standard formula | Arginine-enhanced formula | 7d (≥ 16 mo for survival) |
| De Luis 32 | 2002 | RCT | 47 (24-23) | / | 22 (± 12) | Standard formula | Arginine-enhanced formula | 4d postoperatively and 3mo post-discharge for mortality |
| De Luis 31 | 2003 | RCT | 36 (18-18) | / | 20 | Standard formula | Enteral diet supplemented with arginine and fibre | 5d |
| De Luis 35 | 2004 | RCT | 90 (45-45) | / | ≥ 10 | No support | Glutammine enriched | 14d |
| De Luis 34 | 2005 | RCT | 29 (14-15) | / | 20 | Isocaloric, isonitrogenous enteral formula | Arginine-enhanced formula | 6d |
| De Luis 17 | 2007 | RCT | 72 (35-37) | / | 16 (± 9) | Isocaloric, isonitrogenous enteral formula | Arginine-enhanced formula | Until hospital discharge |
| Casas Rodera 1 | 2008 | RCT | 29 (14-15) | / | 14.5 (± 8) | Standard formula | Arginine, RNA and omega-3 fatty acids (Impact, Nestle) | 14d |
| Sorensen 21 | 2009 | RCT | 15 (8-7) | 7 | 7 | Standard formula | Impact recover oral drink or Impact Glutamine tube feeding | 29d |
| De Luis 19 | 2009 | RCT | 72 (38-34) | / | ≥ 10 | Isocaloric, isonitrogenous enteral formula | Arginine, RNA and omega-3 fatty acids (Impact, Nestle) | 10d |
| Felekis 24 | 2010 | RCT | 40 (20-20) | 5 | 8 | Enteral nutrison (Nutricia) | Arginine, RNA and omega-3 fatty acids (Impact, Nestle) | 8d |
| Ghosh 30 | 2012 | RCT | 57 (28-29) | 5 | 7 | Standard formula | Arginine-enhanced formula | 30d |
| Turnock 28 | 2013 | RCT | 8 (4-4) | 5 | ≥ 5 | Standard formula | Arginine, RNA and omega-3 fatty acids (Impact, Nestle) | Until hospital discharge |
| Falewee 25 | 2014 | RCT | 205 (141-64) | 7 | 7-15 | Standard formula | Arginine, RNA and omega-3 fatty acids (Impact, Nestle) | 90d |
| De Luis 18 | 2014 | RCT | 80 (42-40) | / | ≥ 10 | Isocaloric, isonitrogenous enteral formula | Arginine-enhanced formula | 10d |
| Hanai 29 | 2018 | RCT | 27 (13-14) | 14 | 15 | No support | EPA-containing nutritional supplement | 14d |
| Jantharapattana 22 | 2020 | RCT | 62 (31-31) | 7 | 14 | Standard formula | EPA-containing nutritional supplement | Until hospital discharge |
| Sittitrai 23 | 2021 | RCT | 116 (60-56) | 7 | / | Standard formula | Immune-enhancing diet | 15d |
| Legend: RCT: randomised control trial; d: days; mo: months; N: number of patients; I: patients treated by immunonutrition; C: controls; EPA: eicosapentaneoic acid.. | ||||||||
| Article | Year | Number of patients | Mean age | Gender (M:F) | |||
|---|---|---|---|---|---|---|---|
| Immunonutrition | Control | Immunonutrition | Control | Immunonutrition | Control | ||
| Snyderman 20 | 1999 | 82 | 47 | 63 ± 9.8 | 61 ± 11.7 | 63:19 | 32:15 |
| Riso 26 | 2000 | 23 | 21 | 60.8 ± 9.1 | 63.2 ± 5.7 | 21:2 | 18:3 |
| Van Bokhorst 27 | 2000 | 17 | 15 | 59 ± 12 | 60 ± 8 | 12:5 | 7:8 |
| De Luis 32 | 2002 | 23 | 24 | 63.1 ± 12.7 | 59.3 ± 10.5 | 2:21 | 3:21 |
| De Luis 31 | 2003 | 18 | 18 | 63.1 ± 12.7 | 59.3 ± 10.5 | 1:17 | 1:27 |
| De Luis 35 | 2004 | 45 | 45 | 60.2 ± 12.5 | 60.6 ± 11.5 | 3:42 | 3:42 |
| De Luis 34 | 2005 | 14 | 15 | 60.7 ± 11.6 | 62.9 ± 11.6 | 2:12 | 3:12 |
| De Luis 17 | 2007 | 35 | 37 | 62.1 ± 12 | 61.5 ± 11 | 4:31 | 3:34 |
| Casas Rodera 1 | 2008 | 14 | 15 | 50 ± 13.7 | 54.2 ± 13 | 14:0 | 15:0 |
| Sorensen 21 | 2009 | 8 | 7 | 58.9 ± 7.4 | 61.9 ± 8.5 | 30:8 | 27:7 |
| De Luis 19 | 2009 | 38 | 34 | 63.1 ± 13 | 61.2 ± 9.9 | 8:0 | 7:0 |
| Felekis 24 | 2010 | 20 | 20 | 61 ± 3.8 | 63.2 ± 3.9 | 18:2 | 18:2 |
| Ghosh 30 | 2012 | 28 | 29 | 62 (57-65) | 60 (53-66) | 24:4 | 26:3 |
| Turnock 28 | 2013 | 4 | 4 | 51.2 (28-68) | 47.2 (17-79) | 3:1 | 3:1 |
| Falewee 25 | 2014 | 105 | 104 | 59 ± 9.7 | 59.5 ± 9.6 | 87:18 | 86:18 |
| De Luis 18 | 2014 | 42 | 40 | 65.5 ± 12.2 | 63.6 ± 10.5 | 37:5 | 35:5 |
| Hanai 29 | 2018 | 13 | 14 | 61.5 (45-77) | 66.1 (47-76) | 8:5 | 8:6 |
| Jantharapattana 22 | 2020 | 31 | 31 | 55.2 ± 13.5 | 59.5 ± 13.4 | 24:7 | 26:5 |
| Sittitrai 23 | 2021 | 60 | 56 | 57.3 ± 9.6 | 55 ± 9 | 41:19 | 35:21 |
References
- Casas-Rodera P, Gómez-Candela C, Benítez S. Immunoenhanced enteral nutrition formulas in head and neck cancer surgery: a prospective, randomized clinical trial. Nutr Hosp. 2008;23:105-110.
- Bray F, Ferlay J, Soerjomataram I. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. doi:https://doi.org/10.3322/caac.21492
- Alshadwi A, Nadershah M, Carlson E. Nutritional considerations for head and neck cancer patients: a review of the literature. J Oral Maxillofac Surg. 2013;71:1853-1860. doi:https://doi.org/10.1016/j.joms.2013.04.028
- Vander Poorten V, Uyttebroek S, Robbins K. Perioperative antibiotics in clean-contaminated head and neck surgery: a systematic review and meta-analysis. Adv Ther. 2020;37:1360-1380. doi:https://doi.org/10.1007/s12325-020-01269-2
- Dedivitis R, Aires F, Cernea C. Pharyngocutaneous fistula after total laryngectomy: systematic review of risk factors. Head Neck. 2015;37:1691-1697. doi:https://doi.org/10.1002/hed.23804
- Wang M, Xun Y, Wang K. Risk factors of pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2020;277:585-599. doi:https://doi.org/10.1007/s00405-019-05718-9
- Di Carlo V, Gianotti L, Balzano G. Complications of pancreatic surgery and the role of perioperative nutrition. Dig Surg. 1999;16:320-326. doi:https://doi.org/10.1159/000018742
- Wu G, Zhang Y, Wu Z. Modulation of postoperative immune and inflammatory response by immune-enhancing enteral diet in gastrointestinal cancer patients. World J Gastroenterol. 2001;7:357-362. doi:https://doi.org/10.3748/wjg.v7.i3.357
- Zhang Y, Gu Y, Guo T. Perioperative immunonutrition for gastrointestinal cancer: a systematic review of randomized controlled trials. Surg Oncol. 2012;21:E87-E95. doi:https://doi.org/10.1016/j.suronc.2012.01.002
- Heyland D, Novak F, Drover J. Should immunonutrition become routine in critically ill patients? A systematic review of the evidence. JAMA. 2001;286:944-953. doi:https://doi.org/10.1001/jama.286.8.944
- Howes N, Atkinson C, Thomas S. Immunonutrition for patients undergoing surgery for head and neck cancer. Cochrane Database Syst Rev. 2018;8. doi:https://doi.org/10.1002/14651858.CD010954.pub2
- Vidal-Casariego A, Calleja-Fernández A, Villar-Taibo R. Efficacy of arginine-enriched enteral formulas in the reduction of surgical complications in head and neck cancer: a systematic review and meta-analysis. Clin Nutr. 2014;33:951-957. doi:https://doi.org/10.1016/j.clnu.2014.04.020
- Bertazzoni G, Testa G, Tomasoni M. The Enhanced Recovery After Surgery (ERAS) protocol in head and neck cancer: a matched-pair analysis. Acta Otorhinolaryngol Ital. 2022;42:325-333. doi:https://doi.org/10.14639/0392-100X-N2072
- Coyle M, Main B, Hughes C. Enhanced Recovery After Surgery (ERAS) for head and neck oncology patients. Clin Otolaryngol. 2016;41:118-126. doi:https://doi.org/10.1111/coa.12482
- Kiong K, Vu C, Yao C. Enhanced Recovery After Surgery (ERAS) in head and neck oncologic surgery: a case-matched analysis of perioperative and pain outcomes. Ann Surg Oncol. 2021;28:867-876. doi:https://doi.org/10.1245/s10434-020-09174-2
- Page M, McKenzie J, Bossuyt P. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. doi:https://doi.org/10.1136/bmj.n71
- de Luis D, Izaola O, Cuellar L. Clinical and biochemical outcomes after a randomized trial with a high dose of enteral arginine formula in postsurgical head and neck cancer patients. Eur J Clin Nutr. 2007;61:200-204. doi:https://doi.org/10.1038/sj.ejcn.1602515
- de Luis D, Izaola O, de la Fuente B. Effect of L-arginine supplementation on insulin resistance and adipocitokines levels in head and neck cancer non diabetic patients after surgery. Nutr Hosp. 2014;30:870-875. doi:https://doi.org/10.3305/nh.2014.30.4.7864
- De Luis D, Izaola O, Cuellar L. High dose of arginine enhanced enteral nutrition in postsurgical head and neck cancer patients. A randomized clinical trial. Eur Rev Med Pharmacol Sci. 2009;13:279-283.
- Snyderman C, Kachman K, Molseed L. Reduced postoperative infections with an immune-enhancing nutritional supplement. Laryngoscope. 1999;109:915-921. doi:https://doi.org/10.1097/00005537-199906000-00014
- Sorensen D, McCarthy M, Baumgartner B. Perioperative immunonutrition in head and neck cancer. Laryngoscope. 2009;119:1358-1364. doi:https://doi.org/10.1002/lary.20494
- Jantharapattana K, Orapipatpong O. Efficacy of EPA-enriched supplement compared with standard formula on body weight changes in malnourished patients with head and neck cancer undergone surgery: a randomized study. Head Neck. 2020;42:188-197. doi:https://doi.org/10.1002/hed.25987
- Sittitrai P, Ruenmarkkaew D, Booyaprapa S. Effect of a perioperative immune-enhancing diet in clean-contaminated head and neck cancer surgery: a randomized controlled trial. Int J Surg. 2021;93. doi:https://doi.org/10.1016/j.ijsu.2021.106051
- Felekis D, Eleftheriadou A, Papadakos G. Effect of perioperative immuno-enhanced enteral nutrition on inflammatory response, nutritional status, and outcomes in head and neck cancer patients undergoing major surgery. Nutr Cancer. 2010;62:1105-1112. doi:https://doi.org/10.1080/01635581.2010.494336
- Falewee M, Schilf A, Boufflers E. Reduced infections with perioperative immunonutrition in head and neck cancer: exploratory results of a multicenter, prospective, randomized, double-blind study. Clin Nutr. 2014;33:776-784. doi:https://doi.org/10.1016/j.clnu.2013.10.006
- Riso S, Aluffi P, Brugnani M. Postoperative enteral immunonutrition in head and neck cancer patients. Clin Nutr. 2000;19:407-412. doi:https://doi.org/10.1054/clnu.2000.0135
- Van Bokhorst-de Van der Schuer M, Langendoen S, Vondeling H. Perioperative enteral nutrition and quality of life of severely malnourished head and neck cancer patients: a randomized clinical trial. Clin Nutr. 2000;19:437-444. doi:https://doi.org/10.1054/clnu.2000.0148
- Turnock A, Calder P, West A. Perioperative immunonutrition in well-nourished patients undergoing surgery for head and neck cancer: evaluation of inflammatory and immunologic outcomes. Nutrients. 2013;5:1186-1199. doi:https://doi.org/10.3390/nu5041186
- Hanai N, Terada H, Hirakawa H. Prospective randomized investigation implementing immunonutritional therapy using a nutritional supplement with a high blend ratio of-3 fatty acids during the perioperative period for head and neck carcinomas. Jpn J Clin Oncol. 2018;48:356-361. doi:https://doi.org/10.1093/jjco/hyy008
- Ghosh S, Dempsey G, Skelly R. A double blind, randomised, placebo controlled, feasibility phase III clinical trial of peri-operative immune-enhancing enteral nutrition in patients undergoing surgery for advanced head and neck cancer. e-SPEN Journal. 2012;7:E107-E114. doi:https://doi.org/10.1016/j.clnme.2011.12.001
- de Luis D, Izaola O, Cuellar L. Effect of c-reactive protein and interleukins blood levels in postsurgery arginine-enhanced enteral nutrition in head and neck cancer patients. Eur J Clin Nutr. 2003;57:96-99. doi:https://doi.org/10.1038/sj.ejcn.1601512
- de Luis D, Aller R, Izaola O. Postsurgery enteral nutrition in head and neck cancer patients. Eur J Clin Nutr. 2002;56:1126-1129. doi:https://doi.org/10.1038/sj.ejcn.1601458
- Wilson A, Treasure T, Sturridge M. A scoring method (ASEPSIS) for postoperative wound infections for use in clinical trials of antibiotic prophylaxis. Lancet. 1986;1:311-313. doi:https://doi.org/10.1016/s0140-6736(86)90838-x
- de Luis D, Arranz M, Aller R. Immunoenhanced enteral nutrition, effect on inflammatory markers in head and neck cancer patients. Eur J Clin Nutr. 2005;59:145-147. doi:https://doi.org/10.1038/sj.ejcn.1602034
- de Luis D, Izaola O, Cuellar L. Randomized clinical trial with an enteral arginine-enhanced formula in early postsurgical head and neck cancer patients. Eur J Clin Nutr. 2004;58:1505-1508. doi:https://doi.org/10.1038/sj.ejcn.1601999
- Kattar N, Wang S, Trojan J. Enhanced recovery after surgery protocols for head and neck cancer: systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2023;168:593-601. doi:https://doi.org/10.1177/01945998221082541
- Grammatica A, Piazza C, Paderno A. Free flaps in head and neck reconstruction after oncologic surgery: expected outcomes in the elderly. Otolaryngol Head Neck Surg. 2015;152:796-802. doi:https://doi.org/10.1177/0194599815576905
- Matos L, Sanabria A, Robbins K. Management of older patients with head and neck cancer: a comprehensive review. Adv Ther. 2023;40:1957-1974. doi:https://doi.org/10.1007/s12325-023-02460-x
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 2017 times
- PDF downloaded - 607 times



