Laryngology
Vol. 45: Issue 2 - April 2025
Validation of the Comparative pre/post-treatment Self-Assessment of Dysphonia (CSAD) questionnaire: preliminary results
Abstract
Objective. This study aims to show preliminary results of the validation the Comparative pre/post-treatment Self-Assessment of Dysphonia (CSAD) questionnaire in assessing vocal quality and phonatory fatigue following treatment for dysphonia.
Methods. A retrospective analysis was conducted on 51 patients who underwent phonosurgery for various vocal diseases. Patients completed the CSAD questionnaire post-treatment, alongside the Voice Handicap Index (VHI-10) administered before and after treatment. Correlation analyses were performed between CSAD scores and differences in pre- and post-treatment VHI-10 scores.
Results. The CSAD demonstrated simplicity and ease of interpretation, requiring no pre-treatment administration. Despite its streamlined nature, it exhibited a satisfactory level of correlation with post-treatment VHI-10 scores, indicating its effectiveness in evaluating treatment outcomes for dysphonia.
Conclusions. The CSAD emerges as a simple yet effective tool for self-assessing vocal quality and phonatory fatigue after treatment in patients with dysphonia. Its straightforwardness and post-treatment administration make it a manageable and valuable addition to clinical practice, streamlining assessment processes without compromising accuracy.
Introduction
Self-assessment of dysphonia is considered an essential component in dysphonia assessment 1,2, as it is correlated with both instrumental and perceptual evaluations. This integrated approach allows for a comprehensive evaluation of dysphonia 3. The Voice Handicap Index (VHI) is a widely used self-assessment tool for dysphonia in adult populations, available in both a 30-item version (VHI) 4 and an abbreviated 10-item version (VHI-10) 5. These questionnaires have been translated and validated in several languages, including Italian 6-11. The development of brief and effective questionnaires, such as the VHI-10 12,13, is essential in the clinical evaluation of dysphonia 14. A comprehensive evaluation of dysphonia necessitates a significant amount of time to perform multidimensional assessments. Proposed and validated VHI versions include CVHI-10 for individuals under 16 15 and CVHI-10-P for parents of children with dysphonia 16.
It is important to note that while instrumental assessments offer enhanced sensitivity in diagnosis of dysphonia, self-assessments address an additional dimension and should always be included in treatment plans for dysphonia 17.
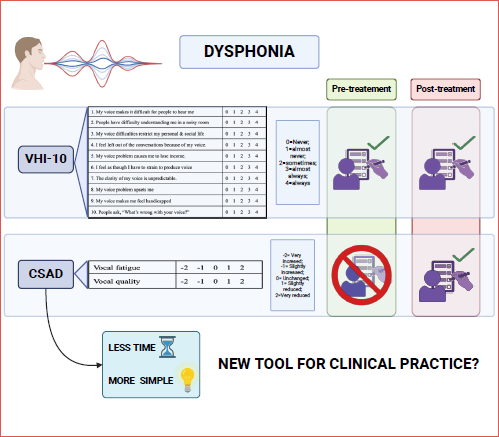
In 2002, the Italian Society of Phoniatrics and Logopedics (SIFEL) introduced their own dysphonia assessment protocol, which incorporates the VHI-10 and the Comparative pre/post-treatment Self-Assessment of Dysphonia (CSAD) for vocal fatigue and vocal quality 2.
The CSAD is a self-assessment tool for dysphonia that provides information on the efficacy of medical or surgical interventions. The CSAD questionnaire is administered solely after treatment of dysphonia, unlike the VHI or VHI-10, which require assessment both before and after treatment. CSAD prompts patients to indicate whether their voice fatigue and voice quality have improved, remained unchanged, or worsened following treatment. A score of +1 is assigned for slight improvement, while a score of +2 indicates significant improvement. Similarly, a negative score is assigned if the patient perceives a deterioration in phonatory fatigue and vocal quality (-1 for slight reduction, -2 for significant reduction). If there is no improvement noted after treatment, a score of 0 is given. Evaluations are conducted for both question 1 (Voice Fatigue ‘La fatica nel parlare è...’ - CSADf) and question 2 (Voice Quality ‘La qualità della mia voce è...’ - CSADq).
The objective of this study is to evaluate the efficacy of the CSAD for self-assessment of vocal fatigue and vocal quality, and to provide a preliminary validation of this instrument. To achieve this, the changes in VHI-10 questionnaire scores administered to patients before and after treatment were compared with scores obtained from the CSAD completed by the same patients after treatment. This supports the validation of the CSAD for the assessment of vocal fatigue and vocal quality.
Materials and methods
A retrospective study was conducted on 51 patients who underwent phonosurgery for vocal diseases within the past 2 years at the ENT Unit of the “M. Bufalini” Hospital in Cesena, Italy. Patients were treated by the same surgeons with over 10 years of experience in phonosurgery. The age of patients ranged from 18 to 80 years, with an average age of 50.9 years (± 14). Of the 51 patients included in the study, 27 were males (52.9%) and 24 were females (47.1%).
The study involved patients with benign vocal fold diseases, such as unilateral vocal fold paralysis, vocal fold hypotrophy, posterior laryngeal granuloma, angiomatous vocal fold polyp, Reinke’s oedema and papillomatosis (Tab. I).
Prior and after phonosurgery, patients were asked to complete forms containing the Italian version of the VHI-10 (Fig. 1) and CSAD (Fig. 2), respectively, in accordance with the SIFEL protocol. The scores for each question on the CSAD were compared with the difference between post- and pre-treatment scores on the VHI-10.
Statistical analysis was carried out using R Statistical Software (v4.3.2; R Core Team, Vienna, Austria). The internal consistency of the CSAD was assessed using Cronbach’s a coefficient. For each VHI-10 questionnaire, the difference (ΔVHI-10) between post- and pre-treatment values was obtained in order to compare the outcomes of VHI-10 and each question of the CSAD (Voice Fatigue – CSADf - and Voice Quality - CSADq). The normality of the distributions was assessed with the Kolmogorov-Smirnov test. To investigate concurrent validity of the CSAD, the correlations between ΔVHI-10 and CSAf scores and between ΔVHI-10 and CSADq scores were studied via the Spearman rank-order correlation coefficient (rs) and the coefficient of determination (r2). Interpretation guidelines for the r statistics were provided by Frey et al. 20. An alpha of 0.05 was considered for statistical procedures.
Results
Cronbach’s coefficient value for the CSAD was very satisfactory (α = 0.86), indicating an excellent balance between high internal consistency and minimal redundancy of items. Mean CSAD (CSADf and CSADq) values and mean ΔVHI-10 values are shown in Table I. The Spearman rank order correlation coefficient was rs = 0.55 (p < 0.0001) for CSADf and ΔVHI-10 and rs = 0.56 (p < 0.0001) for CSADq and ΔVHI-10, suggesting a good level of correlation between the CSAD post-treatment scores and the differences between pre- and post-treatment VHI-10 scores 20. The coefficient of determination was r2 = 0.30 for CSADf and r2 = 0.31 for CSADq, indicating that 30% and 31% of the variance in mean ΔVHI-10 was accounted for, respectively (Tab. II).
Discussion
During the comprehensive assessment of dysphonia, self-evaluation is integrated with perceptual and instrumental assessments 1,2. Together, these evaluations enable clinicians to obtain a thorough and holistic understanding of dysphonia 3. The VHI is the most commonly utilised questionnaire globally, both in clinical practice and scientific research, for self-assessment of dysphonia in adult patients. There are two versions of the VHI: the original extended version, which comprises 30 items and was introduced by Jacobson et al. in 1997 (VHI-30) 4, and a shortened version proposed by Rosen et al. in 2004 (VHI-10) 5. Both versions have been translated into various languages, including Italian, and have undergone validation processes 6-11. The VHI-10 offers the advantage of quicker administration compared to the extended version, with only a minor loss of information in comparison to the VHI-30 7.
The VHI-30 and VHI-10 are self-assessment tools for dysphonia in adult patients and are not recommended for use in younger patients. To overcome this limitation, the Pediatric Voice Handicap Index (pVHI) was developed in 2006 by Zur et al. 17. The pVHI is an instrument that can be used to assess the well-being of children with dysphonia. It is administered to the child’s parents and consists of 23 questions divided into three domains: functional (7 questions), emotional (7 questions), and physical (9 questions). Parents are invited to respond to these questions using a 5-point scale ranging from 0 (never) to 4 (always). The pVHI has been translated and validated in several languages, including Italian 18. A potential limitation of this questionnaire is that it is completed by parents and not by the child. However, to address this limitation, Ricci Maccarini et al. introduced the CVHI-10 in 2013, which is a modified version of the VHI-10 designed for dysphonic patients under the age of 16 19. Additionally, in 2016, Ricci Maccarini et al. developed and validated the CVHI-10-P, which is specifically intended for parents of children with dysphonia.
In 2002, the Italian Society of Phoniatrics and Logopedics (SIFEL) introduced its own dysphonia assessment protocol (Fig. 1), which incorporates the VHI-10 and the CSAD regarding vocal fatigue and vocal quality 2.
Having a concise questionnaire for patient administration is crucial in everyday clinical practice, given the diminishing time available for thorough clinical examinations. The CSAD presents an even more streamlined alternative to the VHI-10, comprising only 2 questions, each offering 5 possible responses, thereby enhancing efficiency in administration. While the simplification of items compared to the VHI-10 limits the spectrum of conditions explored, resulting in a suboptimal correlation coefficient, our findings still demonstrate a satisfactory level of correlation between post-treatment CSAD scores and differences in pre- and post-treatment VHI-10 scores. Therefore, it is suggested that the CSAD be included in the multidimensional assessment of the dysphonic patient as it enables a reliable assessment of treatment efficacy.
Another advantage of CSAD is its simplicity for patient comprehension. Patients are asked to indicate whether the treatment has led to improvements in vocal quality and vocal fatigue, categorising improvements as high or mild, and likewise for worsened conditions. If the treatment yields no discernible benefits, patients can indicate that their voice is unchanged. The simplicity of CSAD not only reduces the time required to complete the questionnaire, but also assists in data collection, thus providing additional support to clinicians.
Furthermore, it is worth noting that CSAD can be administered after treatment, unlike the VHI (both VHI-30 and VHI-10), which requires pre- and post-treatment evaluations. This feature has the potential to streamline data collection in clinical and research settings, while also reducing the time required for use.
Conclusions
The CSAD is an exceedingly simple and straightforward questionnaire, offering ease of interpretation, which facilitates efficient self-assessment of vocal quality and phonatory fatigue after treatment. Unlike other assessments, it does not require administration before treatment. These features make the CSAD a simple yet effective tool for the evaluation of patients with dysphonia after treatment, offering manageability without compromising its efficacy.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
GDP, EN: data collection, analysis; EN: statistical analysis; ARC, GDP, EN: writing original draft; ARC, FM, GDP, MF, EN, MM, MS: reviewing and editing; ARC, MS: conceptualisation, supervision.
Ethical consideration
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: August 15, 2024
Accepted: February 2, 2025
Figures and tables
Figure 1. The dysphonia assessment protocol, which was introduced in 2002 by the Italian Society of Phoniatrics and Speech Therapy (SIFEL), incorporates the VHI-10 and the Comparative pre/post-treatment Self-Assessment of Dysphonia (CSAD) for vocal fatigue and vocal quality.
Figure 2. The English version of CSAD.
| Age (y) | Gender | Pathology | Surgical procedure |
|---|---|---|---|
| 54 | M | SULCUS/VERGETURE | INJECTION LARYNGOPLASTY (HYALURONIC ACID) |
| 40 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 46 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 46 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 60 | M | VOCAL FOLD HYPOTROPHY | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 58 | F | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 28 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 50 | M | POSTERIOR LARYNGEAL GRANULOMA | KTP LASER PHOTOCOAGULATION (FEPS) |
| 54 | F | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 41 | M | VOCAL FOLD HYPOTROPHY | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 67 | F | REINKE’S OEDEMA | KTP LASER PHOTOCOAGULATION (FEPS) |
| 73 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 59 | M | VOCAL FOLD HYPOTROPHY | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 70 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 50 | M | SULCUS/VERGETURE | INJECTION LARYNGOPLASTY (HYALURONIC ACID) |
| 48 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 40 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 42 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 71 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 40 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 26 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 34 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 43 | F | SULCUS/VERGETURE | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 57 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 48 | F | REINKE’S OEDEMA | KTP LASER PHOTOCOAGULATION (FEPS) |
| 48 | F | VOCAL FOLD HYPOTROPHY | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 63 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 54 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 28 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 59 | F | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 52 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 56 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 54 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 40 | M | PAPILLOMATOSIS | KTP LASER PHOTOCOAGULATION (FEPS) |
| 45 | M | ANGIOMATOUS VOCAL FOLD POLYP | KTP LASER PHOTOCOAGULATION (FEPS) |
| 50 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 63 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 24 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 63 | F | PAPILLOMATOSIS | KTP LASER PHOTOCOAGULATION (FEPS) |
| 30 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 42 | M | PAPILLOMATOSIS | KTP LASER PHOTOCOAGULATION (FEPS) |
| 62 | F | REINKE’S OEDEMA | KTP LASER PHOTOCOAGULATION (FEPS) |
| 17 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 55 | F | SULCUS/VERGETURE | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 44 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 60 | F | REINKE’S OEDEMA | KTP LASER PHOTOCOAGULATION (FEPS) |
| 76 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 80 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 55 | F | REINKE’S OEDEMA | KTP LASER PHOTOCOAGULATION (FEPS) |
| 74 | F | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| 57 | M | VOCAL FOLD PARALYSIS | INJECTION LARYNGOPLASTY (AUTOLOGOUS FAT) |
| FEPS: flexible endoscopic phono-surgery; KTP: potassium titanyl phosphate; F: female; M: male. | |||
| Parameter | Mean score ± SD | Spearman rank-order correlation coefficient (rs) | |
|---|---|---|---|
| CSAD question 1 | ΔVHI-10 | 20.92 ± 8.84 | 0.55† |
| CSADf | 1.8 ± 0.38 | ||
| CSAD question 2 | ΔVHI-10 | 20.92 ± 8.84 | 0.56† |
| CSADq | 1.78 ± 0.41 | ||
| † Significance. | |||
References
- Dejonckere P, Bradley P, Clemente P. A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques. Guideline elaborated by the Committee on Phoniatrics of the European Laryngological Society (ELS). Eur Arch Otorhinolaryngol. 2001;258:77-82. doi:https://doi.org/10.1007/s004050000299
- Lechien J, Geneid A, Bohlender J. Consensus for voice quality assessment in clinical practice: guidelines of the European Laryngological Society and Union of the European Phoniatricians. Eur Arch Otorhinolaryngol. 2023;280:5459-5473. doi:https://doi.org/10.1007/s00405-023-08211-6
- Amir O, Tavor Y, Leibovitzh T. Evaluating the validity of the Voice Handicap Index-10 (VHI-10) among Hebrew speakers. Otolaryngol Head Neck Surg. 2006;135:603-607. doi:https://doi.org/10.1016/j.otohns.2006.06.1252
- Jacobson B, Johnson A, Grywalski C. The Voice Handicap Index (VHI): development and validation. Am J Speech Lang Pathol. 1997;6:66-70. doi:https://doi.org/10.1044/1058-0360.0603.66
- Rosen C, Lee A, Osborne J. Development and validation of the voice handicap index-10. Laryngoscope. 2004;114:1549-1556. doi:https://doi.org/10.1097/00005537-200409000-00009
- Schindler A, Ottaviani F, Mozzanica F. Cross-cultural adaptation and validation of the Voice Handicap Index into Italian. J Voice. 2010;24:708-714. doi:https://doi.org/10.1016/j.jvoice.2009.05.006
- Forti S, Amico M, Zambarbieri A. Validation of the Italian Voice Handicap Index-10. J Voice. 2014;28:263.e17-263.e22. doi:https://doi.org/10.1016/j.jvoice.2013.07.013
- Behlau M, Alves Dos Santos Lde M, Oliveira G. Cross-cultural adaptation and validation of the voice handicap index into Brazilian Portuguese. J Voice. 2011;25:354-359. doi:https://doi.org/10.1016/j.jvoice.2009.09.007
- Malki K, Mesallam T, Farahat M. Validation and cultural modification of Arabic voice handicap index. Eur Arch Otorhinolaryngol. 2010;267:1743-1751. doi:https://doi.org/10.1007/s00405-010-1296-x
- Lam P, Chan K, Ho W. Cross-cultural adaptation and validation of the Chinese Voice Handicap Index-10. Laryngoscope. 2006;116:1192-1198. doi:https://doi.org/10.1097/01.mlg.0000224539.41003.93
- Núñez-Batalla F, Corte-Santos P, Señaris-González B. Adaptation and validation to the Spanish of the Voice Handicap Index (VHI-30) and its shortened version (VHI-10). Acta Otorrinolaringol Esp. 2007;58:386-392. doi:https://doi.org/10.1016/S2173-5735(07)70376-9
- Watson N, Oakeshott P, Kwame I. A comparison of the voice handicap index-10 scores between medical and musical theater students. J Voice. 2013;27:129.e21-129.e23. doi:https://doi.org/10.1016/j.jvoice.2012.08.009
- da Costa de Ceballos A, Carvalho F, de Araújo T. Diagnostic validity of Voice Handicap Index-10 (VHI-10) compared with perceptive-auditory and acoustic speech pathology evaluations of the voice. J Voice. 2010;24:715-718. doi:https://doi.org/10.1016/j.jvoice.2009.03.006
- Deary I, Webb A, Mackenzie K. Short, self-report voice symptom scales: psychometric characteristics of the voice handicap index-10 and the vocal performance questionnaire. Otolaryngol Head Neck Surg. 2004;131:232-235. doi:https://doi.org/10.1016/j.otohns.2004.02.048
- Ricci-Maccarini A, De Maio V, Murry T. Development and validation of the children’s voice handicap index-10 (CVHI-10). J Voice. 2013;27:258.e23-258.e28. doi:https://doi.org/10.1016/j.jvoice.2012.10.006
- Ricci-Maccarini A, De Maio V, Murry T. Development and validation of the Children’s Voice Handicap Index-10 for parents. J Voice. 2016;30:120-126. doi:https://doi.org/10.1016/j.jvoice.2014.10.004
- Zur K, Cotton S, Kelchner L. Pediatric Voice Handicap Index (pVHI): a new tool for evaluating pediatric dysphonia. Int J Pediatr Otorhinolaryngol. 2007;71:77-82. doi:https://doi.org/10.1016/j.ijporl.2006.09.004
- Schindler A, Tiddia C, Ghidelli C. Adaptation and validation of the Italian Pediatric Voice Handicap Index. Folia Phoniatr Logop. 2011;63:9-14. doi:https://doi.org/10.1159/000319730
- Hogikyan N, Sethuraman G. Validation of an instrument to measure voice-related quality of life (V-RQOL). J Voice. 1999;13:557-569. doi:https://doi.org/10.1016/s0892-1997(99)80010-1
- Frey L, Botan C, Friedman P. Investigating Communication: An Introduction to Research Methods. Prentice- Hall; 1991.
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 871 times
- PDF downloaded - 193 times



