Rhinology
Vol. 45: Issue 2 - April 2025
Adenoidectomy as day surgery: feasibility and outcomes
Abstract
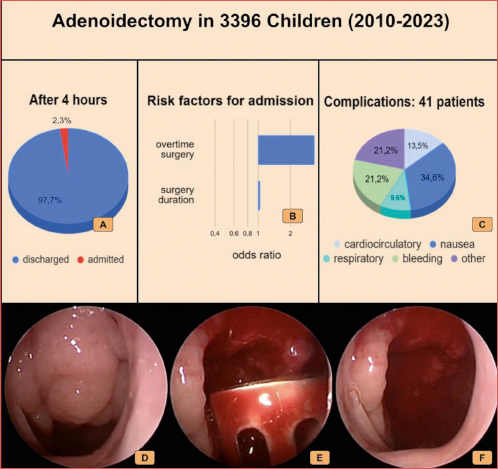
Objectives. Adenoidectomy performed as day surgery is a safe and cost-effective procedure, but patients may be occasionally admitted overnight due to the need for extended care. This study investigates the unplanned admission rate following day surgery adenoidectomy in children.
Methods. Data from 3,396 children who underwent adenoidectomy from 2010 to 2023 were retrospectively collected in a tertiary centre. Inclusion criteria were age > 2 years and ASA score I-II. The study focused on evaluating factors such as age, gender, duration of surgery, surgeon’s experience, adverse events and multiple surgeries. Univariate and multivariate analysis were performed, and ROC curves were built for continuous variables.
Results. The unplanned admission rate was 2.3%, with postoperative nausea/vomiting being the most common complication. Respiratory complications were notably low. Factors associated with unplanned admission at multivariate analysis included the end time of surgery (p < 0.001), surgical duration (p = 0.001) and surgeon’s experience (p < 0.001).
Conclusions. This study confirms the safety and feasibility of adenoidectomy as day surgery in a tertiary centre, with a low unplanned admission rate and infrequent serious complications. Further studies are needed to generalise these findings to different settings and populations.
Introduction
In this century, there has been a trend toward increasing the number of surgical procedures performed on an outpatient or day surgery basis, following the pioneering work of James H. Nicoll 1. However, the specific adoption of day surgery practices for adenoidectomy vary by country and local healthcare policies. The practice of performing adenoidectomy as a day surgery has become more common in recent decades due to advancements in medical technology, anaesthesia and surgical techniques. Over the past few years, as a result of economic pressures combined with targeted research to reduce postoperative complications, adenoidectomy became a standard day surgery procedure 2. Adenoidectomy is included in the list of surgical procedures performed in day surgery, as specified in the agreement between the Ministry of Health and the Regions in 2002, with the relevant indications incorporated in both the National Guideline System document of 2003 and the Italian guidelines of 2008 3.
Shorter waiting times for surgery, lower risk of cross-infection and minimal disruption to routine are just a few examples of advantages to the patient. Last but not least, a further advantage is the reduced period of stay, which is highly recommended for children, because of their psychological vulnerability to illness and hospitalisation 4.
Nowadays adenoidectomy as day surgery, both with and without myringotomy or tympanostomy tube insertion, has been widely regarded to be a safe procedure. The worldwide literature has shown it to be both safe and cost-effective 5.
Even if adenoidectomy is considered a safe procedure, there are instances when patients cannot be discharged from the hospital due to a complication. The primary aim of our study was to assess the unplanned admission rate following adenoidectomy performed as day surgery in children, with a secondary objective to examine the correlation between recorded variables and unplanned admissions.
Materials and methods
Study population and design
A retrospective review of patients who underwent adenoidectomy in day surgery from 2010 to 2023 at a pediatric tertiary-care referral centre was performed.
Inclusion criteria comprised age > 2 years with ASA score I-II, who resided within a 30 km radius on the evening of the procedure.
Exclusion criteria comprised: patients residing beyond a 30 km radius, patients whose families did not offer support for postoperative care, children with obstructive sleep apnoea syndrome, obesity (defined as a body mass index greater than 95th percentile for their age and gender) and congenital or genetic disorders.
Multiple surgery was not an exclusion criteria per se, but patients were excluded if the second surgical procedure was not eligible for day surgery.
The recorded variables included age, gender, surgery duration, end-time of surgery, discharge/unplanned admission, surgeon’s experience (trainee/expert), adverse events (cardiocirculatory complications, respiratory complications, bleeding, postoperative nausea/vomiting, other complications) and multiple surgeries (otolaryngologic surgery/other surgery).
An additional variable named “overtime” was defined for surgical procedures that ended after the scheduled time of the operating theatre session.
Objectives
The main objective of our study was to measure the unplanned admission rate after adenoidectomy performed as day surgery in children.
The secondary objective was to analyse the correlation between the recorded variables and the unplanned admission.
Clinical practice protocol for management of adenoid hypertrophy in our institution
Children were evaluated by the medical team not later than the day before surgery. Informed consent for the operation was obtained from both parents or legal tutors. Parents were informed that the family should resided within a 30 km radius of the hospital, and if patients reside further away, they were advised to stay overnight in a nearby hotel on the evening of the surgery. Families were educated about potential complications including bleeding, nausea, and vomiting, and were instructed to return to the hospital’s emergency department in case of any complications. A leaflet with instructions and possible complications was provided, along with a contact number for assistance.
A premedication with oral midazolam was prescribed if necessary. No preoperative blood or other tests were required. Preoperative fasting was scheduled based on international guidelines 6.
Upon admission to the Day Hospital Unit all patients were re-evaluated to rule out the presence of respiratory tract infection or other contraindications to surgery. In all cases, surgery was performed during the morning operating theatre session (from 8 am to 2 pm). Prevention of postoperative nausea with dexamethasone or ondansetron was administered to all patients.
Adenoidectomy was performed under general anaesthesia with oral intubation. For children below 6 years of age, inhalational induction with sevoflurane was the preferred technique, while for older children a peripheral line was placed before induction with propofol. Fentanyl was administered before intubation to the majority of patients. General anaesthesia was maintained with sevoflurane and intravenous paracetamol was administered at the beginning of the surgery, then every 6 hours.
The adenoidectomy surgical procedure was endoscopic-assisted through the nose. A rigid pediatric 2.7 mm fibre-endoscope (Karl Storz®) was used. Cutting instruments, such as curettes and adenotomes, were employed for transoral adenoid removal, which was carried out under transnasal endoscopic control. This approach ensures the thorough removal of adenoids, including the retro-tubal portion.
The instruments were introduced through the mouth, maintained by a mouth opener, and the endoscope through the nose allowed for control of the removal of the adenoids and prevention of complications such as damage to the Eustachian tubes. The procedure was performed with the patient in a supine position with the head extended.
At the end of the procedure, bleeding control was achieved by applying pressure to the rhinopharynx using cottonoids or gauze. If this was insufficient, intraoperative control was carried out using bipolar forceps through the mouth under endoscopic guidance via the nose. The patient was awakened only after ensuring haemostasis.
Children were allowed to eat and drink as soon as completely awake and without postoperative nausea and vomiting (PONV). Patients were discharged at least 4 hours after admission to the ward if they achieved a Post Anaesthetic Discharge Scoring System (PADSS) 7 score ≥ 9 and after the otolaryngologist checked the oropharynx to ensure there was no active bleeding.
Statistical analysis
Data were summarised with frequencies for categorical data and median interquartile range for continuous non-normally distributed data; confidence intervals were also calculated. Chi square test or Kruskal-Wallis were used to study associations between each variable and unplanned admission. For continuous variables with significant association a receiver operating characteristic (ROC) curve was built and the point with the maximum value of Youden’s index was identified as a cut-off point candidate. A logistic regression model was used to perform multivariate analysis. All analyses were performed with R version 4.2.2, setting alpha at 0.05.
Results
Among the 3,575 eligible cases, a total of 3,396 children who underwent adenoidectomy were analysed; 179 patients were excluded since the “unplanned admission” data was missing. The recorded data are summarised in Table I.
The unplanned admission rate was 2.3% and in one-third of the admitted cases at least one adverse event was recorded.
PONV was the most common complication, while the incidence of severe respiratory complications, defined as laryngospasm, bronchospasm and oxygen desaturation, was as low as 0.15%. Uncontrolled bleeding requiring surgical revision was recorded in 0.3% of patients. The number of missing records regarding adverse events was very high (27%), and for this reason the estimated rate cannot be considered accurate and this variable was excluded from multivariate analysis. Surgery was performed by a resident in 10% of cases, but according to the Italian residency system a consultant was always present in the operating theatre.
The results of univariate and multivariate analysis of the risk factors associated with unplanned admission are summarised in Table II.
Age and gender were not associated with an unplanned admission; at univariate analysis all other factors showed a significant association with the unplanned admission: interestingly, multiple surgeries did not show a significant association at multivariate analysis, suggesting that other factors, like the duration or the end time of surgery, have a largest influence on the admission rate. The operator’s experience was an important risk factor, since for the procedures performed by a trainee surgeon the odds ratio of admission increased more than 3 times compared to procedures performed by an expert surgeon.
The end-time of surgery (as well as “overtime surgery”) showed a significant association with unplanned admissions, but the area under the ROC curve was quite low (0.718), as shown in Figure 1; the area under the ROC curve for the duration of surgery was higher (0.762) and interestingly a cut-off of 29 minutes showed a high sensitivity (0.94) in predicting an unplanned admission.
Discussion
Adenoids are an enlargement of the nasopharyngeal tonsil that can lead to mechanical obstruction and chronic inflammation. Adenoids can cause various local and systemic changes and diseases, impacting the nose and ear, as well as the cardiovascular and respiratory systems, particularly in patients with obstructive sleep apnoea. Adenoid hyperplasia is most prevalent in childhood, typically occurring between the ages of 1 and 6, as the nasopharyngeal tonsil naturally regresses during adolescence.
Adenoidectomy has been shown to markedly enhance the quality of life for both children affected by chronic adenoid hypertrophy as well as their caregivers, as reflected in improved scores across domains such as physical well-being, caregiver concerns, and sleep disturbances 8.
The American Academy of Otolaryngology & Head and Neck Surgery published clinical indicators for adenoidectomy, including recurrent episodes of purulent rhinorrhoea, obstructive sleep apnoea syndrome, chronic otitis media with effusion, and others. These guidelines are endorsed in Germany 9,10. In Italy, national guidelines for adenoidectomy were developed by the Ministry of Health in 2008 3. According to the European Position Paper on Rhinosinusitis and Nasal Polyps published in 2020, adenoidectomy may be considered in certain cases of rhinosinusitis 11. Additionally, adenoidectomy is warranted in children diagnosed with acute otitis media with effusion and significant nasal obstruction 12.
The decision to perform adenoidectomy should be individualised and based on the severity and duration of symptoms, as well as the response to medical therapy. Traditional adenoidectomy, performed by instrumentally scraping the nasopharynx, can benefit from enhanced surgical efficacy through the option of endoscopic monitoring. Alternatives to conventional scraping include electro-surgery, micro-debriding, and radiofrequency surgery, which have shown some advantages, particularly regarding intraoperative blood loss and postoperative complications 13,14. However, a comprehensive review of 20 studies involving 2,329 patients compared 4 common surgical approaches – powered shaver adenoidectomy, plasma field ablation adenoidectomy, curettage adenoidectomy, and suction diathermy adenoidectomy – and revealed no significant differences in operative time, intraoperative blood loss, and incidence of postoperative residual tissue 15-17.
The procedure is performed under general anaesthesia to prevent the inhalation of blood during the intervention. Surgery is quick, and the short duration of general anaesthesia allows for the child to be discharged after approximately 4 hours of observation. Surgical complications such as bleeding or anaesthetic issues like nausea and vomiting can prevent discharge. The absolute risk of adenoidectomy appears small, ranging from 0.21% to 0.4% 18, with our result falling within this range at 0.32%.
The day surgery admission criteria for adenoidectomy, including age > 2 years, ASA score I-II, a family accepting discharge and capable of support for postoperative care with residence within a 30 km radius on the evening of the procedure and exclusion of patients with obstructive sleep apnoea syndrome, allow for same-day discharge. This also results in a lower incidence of respiratory complications in our patient population compared to other studies 19,20. While the reported rates of postoperative respiratory adverse events ranged from 0% to 27.3% 21, in our cohort it was 0.02%.
In a review that integrated findings from 15 studies involving 10,731 patients, an impressive average rate of 96.1% successful same-day discharge was reported 21. Notably, our study indicated a slightly higher percentage, with 97.6% of patients being discharged on the same day. The low admission rate observed in our cohort of patients confirms the feasibility of adenoidectomy as a day surgical procedure. However, our results cannot be generalised to individuals with more comorbidities because patients with ASA score ≥ III are excluded from day surgery in our centre.
The proper selection of patients for day surgery is crucial to prevent overnight hospitalisation after the procedure. Obstructive sleep apnoea syndrome (OSAS) is quite common in children with adenoid hypertrophy: while children with severe OSAS (defined as apnoea/hypopnea index > 9) often needs adenotonsillectomy, adenoidectomy alone may be indicated in patients with adenoid hypertrophy and mild or moderate OSAS. Until 2023 at our institution all children with OSAS of any degree were excluded from day surgery. We recently changed our policy, admitting children older than 3 years, with mild or moderate OSAS and no other comorbidity to day surgery, based on our growing experience and supported by recently published national guidelines 22.
Obese patients were excluded, but overweight children (defined as BMI > 85th percentile) were present in our population. The precise proportion of overweight children was not recorded for the present study, but it was comparable to what reported by a larger epidemiological study performed in our region and was higher than 10% 23.
The end-time of the surgery, as well as “overtime surgery,” often leads to patient admission, more due to logistical issues than clinical ones. In fact, many patients are admitted to regular wards because discharge criteria are fulfilled after closure of the day surgery unit 21. On the other hand, the duration of surgery appears to be a more generalisable criterion in predicting unplanned admission: with a median surgery time of 21 minutes, an increased surgical time (over 24 minutes) represents a significant risk factor, reflecting a more challenging procedure or more difficult bleeding control.
While older children show a higher risk of admission in univariate analysis, this finding was not confirmed in multivariate analysis, where age was a non-significant protective factor. Based on these results, age does not seem to be a contraindication for adenoidectomy as day surgery.
All these considerations can be generalised, at least in centres with a high volume of paediatric surgical procedures performing more than 2,000 procedures per year such as our centre. The significance of unplanned admission in cases performed by trainee surgeons is attributed to the well-known learning curve: the higher the surgeon’s surgical volume, the lower the observed complication rate.
Conclusions
Our data confirms that adenoidectomy performed as day surgery is a safe procedure with a low rate of unplanned admissions and serious complications in experienced centres. Further studies are needed to generalise this evidence to other populations with more comorbidities. In our study, the surgeon’s experience and duration of surgery were the most relevant risk factors for unplanned admission.
Acknowledgements
No contributors met the ancknoledgements criteria.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contributions
ALA, PB, MB: planned the presented study and supervised the work; ALA, FDB, SA, AP, GM: contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript; GM: performed the statistical analysis. All authors discussed the results and contributed to the final manuscript.
Ethical consideration
Written informed consent was obtained from each parent/legal representative for study participation and data publication. Ethics approval for the creation of a retrospective perioperative database for subsequent analysis and publication was asked to the Institutional Ethics Committee (prot. n. 286/2021): it was exempted by our Ethics Committee who stated that approval was under the Hospital Administration competence. Administration’s approval was granted.
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
History
Received: February 1, 2024
Accepted: April 24, 2024
Figures and tables
Figure 1. ROC curve of “end-time of surgery” vs “unplanned admission” and ROC curve of “duration of surgery” vs “unplanned admission”. In both curves the point with the maximum value of the Youden Index is marked. ROC: Receiver operating characteristic; AUC: Area under the ROC curve.
| Overall | 95% CI | Missing records | |
|---|---|---|---|
| N | 3,396 | ||
| Age, yr (median [IQR]) | 5.2 (4-7.5) | 5-5.3 | 56 |
| Males (%) | 2,109 (62.1) | 0 | |
| End-time (median [IQR]) | 10.45 am (9.45-12) | 10.35-10.54 | 344 |
| Overtime n (%) | 53 (1.7) | 1.3-2.2 | 315 |
| Duration (median [IQR]) | 21 min (18-24) | 20-22 | 344 |
| Other surgery n (%) | |||
| Any surgery | 28 (0.8) | 0.6-1.1 | 0 |
| ENT surgery | 21 (0.6) | 0 | |
| Non-ENT surgery | 7 (0.2) | 0 | |
| Surgical trainee n (%) | 347 (10.2) | 9.2-11.3 | 0 |
| Unplanned admission n (%) | 77 (2.3) | 1.8-2.8 | 0 |
| Adverse event n (%) | 41 (1.7) | 1.2-2.2 | 917 |
| Event type n (%) | |||
| Cardiocirculatory n (%) | 7 (13.5*) | ||
| Nausea vomiting n (%) | 18 (34.6*) | ||
| Respiratory n (%) | 5 (9.6*) | ||
| Bleeding n (%) | 11 (21.2*) | ||
| Other n (%) | 11 (21.2*) | ||
| *Calculated with respect to all complications. | |||
| No admission | Unplanned admission | Univariate analysis p value* | Multivariate analysis p value# | Odds Ratio** | |
|---|---|---|---|---|---|
| N | 3,319 | 77 | 2997 | ||
| Age (median [IQR]) | 5.1 (4-7.3) | 6.75 (4.02-9.85 | 0.037 | 0.26 | 0.90 |
| Males (%) | 2,059(62) | 50 (64.9) | 0.069 | 0.8 | 1.03 |
| End-time (median [IQR]) | 11.12 am (10.13-12.18) | 12.27 am (11.38-14.32) | 0.001 | < 0.001 | 1.45 |
| Overtime (%) | 39 (1.3) | 14 (18.2) | < 0.001 | 0.02 | 3.33 |
| Duration (median [IQR]) | 20.8 min (18.2-24) | 30 min (24-36.5) | < 0.001 | 0.001 | 1.05 |
| Other surgery (%) | |||||
| Any surgery | 18 (0.5) | 10(13) | < 0.001 | 0.6 | 0.53 |
| ENT surgery | 11 (0.3) | 10(13) | < 0.001 | ||
| Non-ENT Surgert | 7 (0.2) | 0 (0) | 0.9 | ||
| Surgical trainee (%) | 329 (9.9) | 18 (23.4) | < 0.001 | < 0.001 | 3.51 |
| Adverse Event (%) | 13 (0.4) | 28 (36.6) | < 0.001 | ||
| *Chi square test for categorical variables, Kruskal-Wallis test for continuous non-normal variables; # Logistic regression model; ** Increase in odds ratio when incrementing the predictor by one: calculated by exponentiating the logistic model coefficients. | |||||
References
- Young DG, Carachi R. James H Nicoll, MB, CM Glasg, FRFPS Glasg. Legion of Honour France, father of day surgery. Scott Med J 2006;51:48-50. https://doi.org/10.1258/RSMSMJ.51.1.48
- Patel R, Patel NA, Stoffels G, et al. Adenoidectomy: inpatient criteria study. Am J Otolaryngol 2021;42:102765. https://doi.org/10.1016/j.amjoto.2020.102765
- Marchisio P, Villa MP, Bellussi L, et al. Appropriatezza e sicurezza degli interventi di tonsillectomia e/o adenoidectomia. Linea guida SNLG 15. Minerva Pediatr 2008;60:907-909.
- Colclasure JB, Graham SS. Complications of outpatient tonsillectomy and adenoidectomy: a review of 3,340 cases. Ear Nose Throat J 1990;69:155-160.
- Kishore A, Haider-Ali AM, Geddes NK. Patient eligibility for day case paediatric adenotonsillectomy. Clin Otolaryngol Allied Sci 2001;26:47-49. https://doi.org/10.1046/j.1365-2273.2001.00425.x
- Frykholm P, Disma N, Andersson H, et al. Pre-operative fasting in children: a guideline from the European Society of Anaesthesiology and Intensive Care. Eur J Anaesthesiol 2022;39:4-25. https://doi.org/10.1097/EJA.0000000000001599
- Palumbo P, Tellan G, Perotti B, et al. Modified PADSS (Post Anaesthetic Discharge Scoring System) for monitoring outpatients discharge. Ann Ital Chir 2013;84:661-665.
- Shivnani D, Kobal MR, Raman EV, et al. Impact of chronic adenoid hypertrophy on quality of life index in children and role of adenoidectomy. Indian J Otolaryngol Head Neck Surg 2023;75:3396-3401. https://doi.org/10.1007/s12070-023-04000-z
- Wetmore RF. Surgical management of the tonsillectomy and adenoidectomy patient. World J Otorhinolaryngol Head Neck Surg 2017;3:176-182. https://doi.org/10.1016/j.wjorl.2017.01.001
- Ahmad Z, Krüger K, Lautermann J. et al. Adenoid hypertrophy-diagnosis and treatment: the new S2k guideline. HNO 2023;71(Suppl 1):67-72. https://doi.org/10.1007/s00106-023-01299-6
- Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on rhinosinusitis and nasal polyps 2020. Rhinology 2020;58(Suppl S29):1-464. https://doi.org/10.4193/Rhin20.600
- Simon F, Haggard M, Rosenfeld RM, et al. International consensus (ICON) on management of otitis media with effusion in children. Eur Ann Otorhinolaryngol Head Neck Dis 2018;135:S33-S39. https://doi.org/10.1016/j.anorl.2017.11.009
- Ark N, Kurtaran H, Ugur KS, et al. Comparison of adenoidectomy methods: examining with digital palpation vs. visualizing the placement of the curette. Int J Pediatr Otorhinolaryngol 2010;74:649-651. https://doi.org/10.1016/j.ijporl.2010.03.012
- Yang L, Shan Y, Wang S, et al. Endoscopic assisted adenoidectomy versus conventional curettage adenoidectomy: a meta-analysis of randomized controlled trials. SpringerPlus 2016;5:426. https://doi.org/10.1186/s40064-016-2072-1
- Sun YL, Yuan B, Kong F. Comparison between different approaches applied in pediatric adenoidectomy: a network meta-analysis. Ann Otol Rhinol Laryngol 2023;132:207-216. https://doi.org/10.1177/00034894221081612
- Bhandari N, Don DM, Koempel JA. The incidence of revision adenoidectomy: a comparison of four surgical techniques over a 10-year period. Ear Nose Throat J 2018;97:E5-E9. https://doi.org/10.1177/014556131809700601
- Ferreira MS, Mangussi-Gomes J, Ximendes R, et al. Comparison of three different adenoidectomy techniques in children – Has the conventional technique been surpassed? Int J Pediatr Otorhinolaryngol 2018;104:145-149. https://doi.org/10.1016/j.ijporl.2017.11.012
- MacKeith S, Mulvaney CA, Galbraith K, et al. Adenoidectomy for otitis media with effusion (OME) in children. Cochrane Database Syst Rev 2023;10:CD015252. https://doi.org/10.1002/14651858.CD015252.pub2
- Amoils M, Chang KW, Saynina O, et al. Postoperative complications in pediatric tonsillectomy and adenoidectomy in ambulatory vs inpatient settings. JAMA Otolaryngol Head Neck Surg 2016;142:344-350. https://doi.org/10.1001/jamaoto.2015.3634
- Caetta A, Timashpolsky A, Tominaga SM, et al. Postoperative respiratory complications after adenotonsillectomy in children with obstructive sleep apnea. Int J Pediatr Otorhinolaryngol 2021;148:110835. https://doi.org/10.1016/j.ijporl.2021.110835
- Gowda S, Leong WS, Edafe O. Day-case discharge criteria and safety of children undergoing adenoidectomy and tonsillectomy for obstructive symptoms – A systematic review. Clin Otolaryngol 2022;47:553-560. https://doi.org/10.1111/coa.13946J
- SIAARTI. Buone pratiche sul management anestesiologico dei bambini con Obstructive Sleep Apnoea Syndrome (OSAS). https://www.siaarti.it/news/1950614, Accessed: April 10, 2024.
- Stival C, Lugo A, Barone L, et al. Prevalence and correlates of overweight, obesity and physical activity in italian children and adolescents from Lombardy, Italy. Nutrients 2022;14:2258. https://doi.org/10.3390/nu14112258
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1520 times
- PDF downloaded - 158 times




