Otology
Vol. 45: Issue 3 (Suppl. 1) - June 2025
Surgical options for advanced otosclerosis
Abstract
Objective. Management of advanced otosclerosis (AO) has evolved over the past 20 years with the availability of cochlear implant (CI) in addition to stapes surgery. Both procedures are reliable treatment options for AO with similar success rates and currently there are no standard guidelines regarding the surgical treatment of AO. The aim of this paper is to report the outcomes and complications of a series of patients with AO submitted to CI at our Institution. An extensive review of the literature is also provided.
Methods. The study group was composed of 31 adult patients affected by AO, consecutively submitted to CI at our Institution. Postoperative results and complications were compared to those of a homogeneous control group of adult implanted patients, affected by post-verbal sensorineural hearing loss due to other aetiologies.
Results. Patients in both groups achieved satisfactory results in terms of speech perception in quiet and with background noise after CI, without no significant differences. The rate of complications in the study group was 15%, which is similar to literature reports.
Conclusions. In patients with AO, the decision between stapes surgery and CI must be personalized and well-considered, taking into account the individual characteristics of the patient and the potential risks and benefits of each option.
Introduction
Otosclerosis is a well-known disorder of bone metabolism within the otic capsule. Most patients have conductive hearing loss (HL) and can clearly benefit from stapes surgery. However, a smaller proportion of patients, between 8.9 and 34%, eventually progress to mixed or sensorineural HL (SNHL) 1. House and Sheehy, in 1961, first introduced the term “far advanced otosclerosis” (FAO) to describe patients with absent bone conduction thresholds and air conduction thresholds over 85 dB HL 2. Iurato and colleagues added the “very far advanced otosclerosis” terminology to include those with a “blank audiogram” or immeasurable air and bone conduction thresholds 3. With improvements in audiometric equipment, the definition has changed and currently there is not a clear consensus on the definition to be used. Nowadays, in the era of cochlear implantation (CI), speech discrimination scores are more likely to be used instead of pure-tone thresholds values in the definition of the disease and Lachance et al. used the definition of FAO for cases with otosclerosis and poor discrimination scores 4. Similarly, other authors introduced the term advanced otosclerosis (AO) when referring to otosclerotic patients with SNHL and diminished speech discrimination scores, which falls within the criteria for CI candidacy 1,5.
There are no standard guidelines regarding the rehabilitation of AO: the possible treatment options are no intervention and use of hearing aids (HA), stapedotomy and use of HA, or CI procedure. Each has its advantages, disadvantages, success rates, and complications 4,6-12.
In this paper, we report the results and complications rate of a series of patients with AO submitted to CI procedure at our Institution. The results and complications will be compared to those of a homogeneous control group of adult implanted patients, affected by post-verbal SNHL due to other aetiologies. An extensive review of the literature will also be provided.
Materials and methods
The study group was composed of 31 adult patients affected by AO, consecutively submitted to CI at our Institution, during the period 1998-2022. Patients enrolled in the study gave their informed consent to participate.
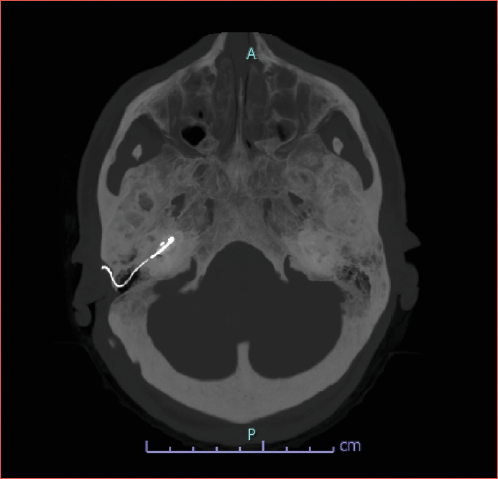
Preoperatively all patients were submitted to a comprehensive audiological evaluation, including medical personal and familial history report, otomicroscopy, pure tone audiometry for air and bone conduction thresholds, impedance audiometry and stapedial reflexes study, speech audiometry, free field warble tone and speech audiometry with and without HA, and a speech perception test 13 without lipreading with HA in quiet and with background noise (signal to noise ratio +10). Patients were also submitted to neuroradiological evaluation using temporal bone high resolution computed tomography (CT) and brain and inner ear magnetic resonance (MR) with contrast. We defined CT findings indicative of otosclerosis as follows: obliterative otosclerosis was identified by ossification of the basal turn of the cochlea, while non-obliterative otosclerosis was characterised by the presence of otospongiotic foci, with the cochlear lumen remaining normal.
Postoperatively, during follow-up visits, all patients were assessed in the usual listening condition by warble tone audiometry in free field and a speech perception test 13 without lipreading in quiet and with background noise (signal to noise ratio +10). The usual listening condition could be with one CI, with bimodal stimulation or with bilateral CI, according to the devices used.
Pure tone audiometry was conducted with the Interacoustics Clinical Audiometer AC40. When measuring the hearing threshold both without and with HA, we assigned a value of 125 dB to any frequency threshold over the maximum output limit of the audiometer (105 dB for 0.25 kHz and 125 dB for 0.5 and 1 kHz, 120 dB for 2 kHz). Any vibrotactile sensation was also excluded.
Speech perception was assessed using a speech perception test in Italian language 13 both before (with HA) and after implantation (in the usual listening condition) in free field, by the same speech therapist in all the patients to avoid bias, with live voice, without lip reading. We evaluated the disyllabic words recognition score using lists of 20 disyllabic Italian words at a level of 65 dB. Performing the test with background noise, we used a signal to noise ratio of +10.
We compared the results of the study group to those of a control group comprising 31 adult patients with post-verbal SNHL from aetiologies other than otosclerosis. These patients received CI at our Institution and were routinely evaluated during follow-up visits. The control group was selected based on the following criteria: age between 39 and 79 years, implanted between 1998 and 2022, normal cochlear anatomy, and absence of cognitive impairment or neuropsychiatric disorders. To ensure the control group had the same age distribution as the study group, we used random selection with SPSS software.
We correlated the speech perception results in quiet and with background noise between study and control groups, both pre- and postoperatively. We also checked if postoperative speech perception results of the study group were correlated with the previous execution of stapedoplasty in the implanted ear, the presence of basal turn ossification due to otospongiosis, electrical stimulation of facial nerve after CI activation and incomplete electrode insertion. Finally, we compared the rate of postoperative complications between the two groups.
Statistical analysis
The normality of the quantitative data was assessed using the Shapiro-Wilk test. As the data did not follow a normal distribution, differences in means were evaluated using the non-parametric Mann-Whitney U test for independent samples. Correlations between continuous, categorical, and dichotomous variables were analysed using the Spearman rank correlation coefficient or the Point-Biserial correlation coefficient. The distribution of quantitative variables across groups was examined using the Independent-Samples Kruskal-Wallis test. For testing the distribution of categorical variables, the Chi-Square or Fisher’s Exact test was used as appropriate. All statistical analyses were conducted using SPSS (IBM SPSS Statistics 26, IBM, New York, NY), with a p value ≤ 0.05 considered as statistically significant.
Results
The study group was composed of 31 patients (33 implants), 18 females and 13 males, with a mean age at implantation of 65.3 years (range, 39-79). The implants used were Cochlear Nucleus CI 24 M in one patient, Cochlear Nucleus CI24RE (CA) in 4, Cochlear Nucleus CI512 in 20, and Cochlear Nucleus CI612 in 7. We used a straight array in one patient implanted at the beginning of our series, when perimodiolar electrodes were not available.
We performed a unilateral CI in 29 patients and a sequential bilateral CI in 2. Ten unilaterally implanted patients use the bimodal stimulation. Fourteen patients had previously undergone stapes surgery in the implanted ear.
Preoperative CT showed an obliterative otosclerosis in 16 ears. Preoperatively the mean disyllabic words recognition score with hearing aids was 30.6% (range, 0-100%) in quiet and 11.7% (range, 0-70%) with background noise. The mean follow-up after surgery was 8.5 years (range, 1-24).
The control group was composed of 31 patients (32 implants), 19 females and 12 males, with a mean age at implantation of 65.1 years (range, 39-79). The implants used were Cochlear Nucleus CI 24 M in one patient, Cochlear Nucleus CI24RE (CA) in 6, Cochlear Nucleus CI512 in 20, and Cochlear Nucleus CI612 in 4 patients (bilateral CI in one patient). We performed a unilateral CI in 30 patients and a sequential bilateral CI in one patient. Ten unilaterally implanted patients use the bimodal stimulation. All the procedures, both for the study and control groups, were performed by the same senior surgeon.
Preoperatively, in the control group the mean disyllabic words recognition score with hearing aids was 23.7% (range, 0-65%) in quiet and 6.6% (range, 0-35%) with background noise. The mean follow-up after surgery was 6.3 years (range, 1-17). No statistically significant difference in preoperative speech recognition scores was present between the study and the control group. Postoperatively in the study group the mean disyllabic words recognition score in the usual listening condition was 69.4% (range, 30-100%) in quiet and 45.7% (range, 0-95%) with background noise. The usual listening condition was with one CI for 19 patients, with bimodal stimulation for 10, and with bilateral CI for 2.
Postoperatively in the control group the mean disyllabic words recognition score in the usual listening condition was 77.7% (range, 50-100%) in quiet and 42.5% (range, 0-85%) with background noise. The usual listening condition was with one CI for 20 patients, with bimodal stimulation for 10, and with bilateral CI for one (Fig. 1).
With regards to complications, in the study group we recorded an incomplete insertion of the array in 2 ears (6%), and a mild gusher that spontaneously resolved intraoperatively in one ear (3%); in no case was there misplacement of the electrode array. Due to postoperative facial nerve stimulation (FNS), it was necessary to modify the implant fitting and to exclude some electrodes in 7 ears. In 2 patients, the fitting changes and the number of excluded electrodes caused a reduction of the outcome. We included only these 2 patients in the calculation of complications (6%). The rate of complications in the study group was 15%. In one patient the electrode array was inserted in the scala vestibuli, due to the obliteration of the scala tympani lumen; this was not included among the complications, as the scala vestibule insertion did not affect the results.
In the control group there was no misplacement or incomplete insertion of the electrode array, gusher, or FNS. There were also no significant differences in postoperative speech perception in quiet and with background noise between the study and control groups.
Within the study group, we found no significant correlation between postoperative word recognition scores, both in quiet and with background noise, and prior stapes surgery, presence of obliterative otosclerosis, and incomplete insertion of the array or FNS.
In Table I the main clinical and audiological features of the patients belonging to the study and control group are reported.
Discussion
Management of AO has evolved over the past 20 years with the availability of CI in addition to stapes surgery 6. Both stapes surgery and CI are reliable treatment options for AO with similar success rates and, currently, there are no standard guidelines regarding the surgical treatment of AO.
In the choice between stapes surgery and CI, the success rate is not the only factor to play a role in the decision; each intervention has specific advantages and disadvantages. Furthermore, many factors must be taken into account besides the audiogram and the air bone gap, such as imaging, contralateral ear hearing level, duration of HL, economic issues, and patient’s preference.
Stapedotomy is a relatively simple, safe, and cost-effective procedure that can accomplish very good results in patients experiencing severe to profound HL due to otosclerosis, who are potentially candidates for CI 4,7,8. In 2014, Van Loon published a systematic review and meta-analysis on stapedotomy in patients with FAO, finding that combining stapedotomy with hearing aid fitting led to good outcomes in a significant number of cases, with 35% of patients achieving a postoperative speech perception score exceeding 80% 7. They also showed that, in comparison to CI procedure, stapes surgery is reportedly less expensive, less complex as it does not need a postoperative rehabilitation programme and offers a more natural quality of sound, allowing a better appreciation of music. Finally, these authors highlighted that stapedotomy can be easily performed under local anaesthesia, making the procedure especially applicable for the elderly and patients with comorbidities 7. However, a feared complication of stapedotomy is an increase of SNHL, which in AO could result in a functionally deaf ear 4.
According to these reasons, some authors suggest considering stapes surgery as the first surgical option in patients with AO, and to reserve CI for cases of failure 7,8.
However, the results after stapedotomy in severe mixed HL are variable and unpredictable. In 2004, our group published the results of 8 patients with FAO submitted to stapes surgery: the results were quite variable, which were satisfactory in 5 patients and poor in the remaining 3 6.
Although stapedotomy in otosclerosis can achieve a stable long-term hearing improvement, patients with otosclerosis may demonstrate a further progression of SNHL that cannot be explained by age alone and that may affect the long-term results after stapedotomy. To date, the exact rate of this progression remains unclear, emphasising the need for studies with longer follow-up after stapedotomy in patients with FAO 7. In this regard, the effects of stapedotomy reported in the literature and reviews are predominantly based on a single postoperative measurement, and most studies lack long-term follow-up 6-8. Four of 8 patients with FAO submitted to stapedotomy, and reported in the above mentioned study 6, during long-term follow-up experienced deterioration of the results and were subsequently submitted to CI (unpublished data).
There are no reportedly reliable prognostic factors for the results after stapedotomy in patients with AO. Age, gender, preoperative pure tone audiometry, and preoperative speech recognition scores do not seem to predict outcomes after stapedotomy 7. Also, the pericochlear extent of otospongiotic foci as seen on preoperative high-resolution CT does not seem to be correlated with postoperative audiologic performance 7.
CI is currently the gold standard for rehabilitation of severe to profound HL and has also been shown to be effective for patients with AO. Historically, the application of a CI to otosclerotic patients was initially met with skepticism, and FAO was considered a contraindication to implant candidacy; nevertheless, in recent years, a growing body of evidence supports the notion that CI is safe and beneficial in AO.
Unlike stapes surgery, CI is an expensive and complex procedure; in the case of otosclerotic patients, it requires experienced surgeons and audiologists, and advanced otosclerosis poses a unique challenge to both the implant team and the patient 10. Intraoperatively, distorted bony anatomy from ossification may necessitate extra-drilling and trauma to the cochlea, and cochlear demineralisation and obliteration may result in the incomplete insertion or misplacement of the electrode array. In this regard, the surgical facility for management of cochlear obstruction and altered bony anatomy is crucial 1. Postoperative complications can develop as a result of the altered current distribution of remodelled bone, leading to higher rates of non-auditory stimulation, mainly FNS 10-12. For these reasons, comprehensive preoperative counselling to discuss the multiple modalities for hearing rehabilitation in AO, including CI, as well as the expected results and possible difficulties is needed 1,11.
In the last few years, a number of review articles and meta-analyses have been published on CI in patients with otosclerosis. It is reported that patients with AO who undergo CI commonly achieve satisfactory speech perception benefits 10,12. Also, the subjectively perceived benefits after implantation, evaluated by patient-reported outcome measures (PROMs) are good, with no significant differences in comparison to patients with different aetiologies of HL 11,14. Lam et al., in a systematic review on this topic, concluded that the hearing outcomes after CI in otosclerosis are generally good, with the majority of patients experiencing good audiometric outcomes and PROMs at 12 months after implantation 11. A systematic review by Kondo et al. reported similar results: they showed improvements in speech recognition scores from CI in patients with FAO similar to general adult CI outcomes 10.
In our aforementioned clinical study, we submitted 5 patients with FAO to CI procedure: in all patients we obtained satisfactory hearing and speech perception results, and 4 of 5 patients were able to have telephone conversations 6.
Conversely, in a clinical study by Wong et al., patients with AO achieved slightly poorer speech perception scores after CI than a control group of non-otosclerotic patients, but the difference between groups was not significant 15.
In agreement with the majority of literature data, the current study found that both the study and control groups achieved satisfactory results in terms of speech perception in quiet and with background noise after CI. Furthermore, outcomes for otosclerotic patients did not differ significantly from those of control patients with HL due to other aetiologies.
Despite generally good hearing and speech perception results, otosclerosis patients undergoing CI report a higher frequency of surgical issues, as well as intra- and postoperative complications. Lam et al., in their paper, noted that a small but significant portion of patients experience poor outcomes post-implantation, often associated with postoperative complications such as FNS 11. Similarly, Kondo et al. reported that otosclerotic patients have higher than usual rates of FNS and partial insertions 10.
Diversity of cochlear anatomy due to ossification should be kept in mind and surgeons need to be prepared for the possibility of obstacles during insertion and the need for an alternative insertion scenario during the procedure 16. The rate of incomplete insertions in patients with AO is about 10% and is higher than what is generally found in implanted adult patients (2%) 10. Although the difficulty of electrode insertion in otosclerosis is often attributed to ossification of the basal turn, a histopathological analysis by Lee et al. showed that cases of partial insertion were associated with cochlear lumen obstruction in only a small number of cases 17. In most cases, cochlear obstruction can be by-passed with the drilling of the basal turn, thus enabling full insertion of the array. Alternatively, for more extended obstructions, scala vestibuli implantation can be a viable option 18. In the literature it has been utilised to variable extents, with the upper limit being in 21% of patients treated by Kabbara et al. 10,19. In cases of scala vestibuli array insertion, most authors did not find any significant difference in postoperative audiological outcomes between scala vestibuli and scala tympani electrode insertions 15,18, although previous studies have shown that full electrode insertions into the scala tympani are associated with superior speech perception 20. In one of the patients of the present study group, a scala vestibuli insertion was executed due to the severity of scala tympany ossification. No significant impact on the postoperative result was recorded 17.
A major concern regarding CI in otosclerotic patients is the possibility of FNS, which is reportedly higher than in the general population of implanted patients 10,12,21,22: in the review by Kondo et al., FNS was the most common non-auditory stimulation and was reported in 18% the cases, which is higher than the 6% rate reported across reviews for all adult CI patients 10. The mechanism underlying this phenomenon seems to be related to the reduced impedance of the otic capsule, which causes electrical currents to shunt through the bone. This leads to an increased current requirement to stimulate auditory nerve fibres and a potential excess current spread to the facial nerve, causing FNS 10. This phenomenon requires to be managed with more frequent adjustments of the electrical map and proper follow-up, with the need to switch off some electrodes, reportedly typically 1-2, but in some cases up to 8, potentially leading to a decrease in the auditory results. Despite this, Kondo et al. reported that studies comparing speech perception outcomes between patients with and without otosclerosis showed poorer results for the former group, but without reaching statistical significance 10. Some authors report that a reduction in audiological outcomes may be correlated with number of electrodes deactivated, but this relationship has yet to be clarified 23. It has been hypothesised that speech perception has an inverse exponential decay relationship to electrode deactivation, such that there is a threshold of stimulation. For instance, significant deterioration in speech perception is seen with a higher number of electrodes deactivated whereas it has not been observed with a smaller number 24,25. Nevertheless, a recent study by Atanasova-Koch et al. also noted that deactivated electrodes did not make a significant difference in speech differentiation 23.
Finally, some studies have suggested the benefit of using perimodiolar electrodes to achieve lower rates of FNS 10; it is estimated that with perimodiolar electrodes, the rate of FNS dropped to nearly 0% 10,12.
Another issue concerning CI procedure in otosclerotic patients is the possibility of progressively decreased performance. This decrease in performance over time can be attributed to several factors, including the unique anatomical and pathological challenges presented by otosclerosis. Some patients may experience a decline in speech recognition scores over time, potentially due to ongoing cochlear changes or suboptimal electrode positioning and insertion depth necessitated by the ossified cochlear structures. The progressive nature of otosclerosis itself can lead to further ossification within the cochlea after implantation. This can impair the performance of the implant due to changes in cochlear structure that affect the transmission of electrical signals from the implant to the auditory nerve. Additionally, there is evidence that otosclerotic patients may experience non-auditory stimulation and FNS more frequently than other cochlear implant users, which can contribute to decreased auditory performance and user discomfort 26.
Structural changes in bone may be progressive, potentially affecting stimulation thresholds, electric charges, pulse widths, stimulation rates, and ultimately, the number of active electrodes, leading to a decrease in outcomes. However, this aspect is not clearly reported in the literature 26. Despite electrode switch-off due to FNS and higher partial insertion rates, CI in AO is generally reported to have comparable speech discrimination rates to normal adult CI 10,12,14.
With regards to other complications, a higher incidence of gusher and lower frequency of postoperative vertigo are reported in this group of patients 10. In our study group, otosclerotic patients had a low rate of complications of 15%, consistent with other literature reports 9,10, even though when compared to the control group, otosclerotic patients had a higher rate of complications. We had incomplete electrode insertion in 6% of otosclerotic patients, which is lower than the percentage reported by Kondo et al. in 2022 10. We observed a gusher in 3% of cases and FNS affecting results in 6% of cases. This is lower than the 18% reported by Kondo et al., possibly due to different criteria for considering FNS as a complication; in fact, we included only cases where FNS reduced speech perception. Furthermore, we used a perimodiolar electrode in a very high proportion of patients, which could explain the low FNS rate.
Teaima et al. in 2023 published an interesting review article, comparing outcomes and side effects in patients with FAO submitted to stapes surgery and CI procedure 9, concluding that results and complications of CI and stapes surgery in FAO patients are different. In most of the studies included in the review, CI was considered highly favourable and more recommended than stapes surgery, while other studies showed no significant difference in postoperative outcomes: CI had a reportedly better mean PTA than stapes surgery and a significantly higher mean for recognition of phrases. On the other hand, stapes surgery had a higher mean for recognition of monosyllables and disyllables than CI 9. With regards to side effects, including dysgeusia and tinnitus, the review showed that postoperative complications were significantly lower in CI (13.6%) than stapes surgery (18.6%). However, vertigo was lower in stapes surgery than in CI. Finally, CI had a significantly lower rate of revision surgery than stapes surgery 9.
Radiological assessment of the severity of otosclerosis has a vital role in preoperative planning, as it may predict difficulties in positioning the electrode or the risk of incomplete insertion, but its value in predicting postoperative hearing outcomes is controversial 11,15. Wong et al. conducted a retrospective study on the role of preoperative radiological assessment of the petrous bone and found that narrowing or signal change in the cochlear lumen has a significant effect on the final electrode position, whereas round window ossification or obstruction did not seem to be relevant 15. Furthermore, they found a strong correlation between preoperative imaging and intraoperative findings for both the cochlea and round window. However, in their study they found that the correlation between postoperative electrode position and preoperative imaging was moderate 15. In addition, they found no significant correlation between hearing outcomes and preoperative radiology, intraoperative findings or postoperative electrode position, concluding that preoperative imaging findings do not predict postoperative speech perception outcomes 15. Similarly, in the current study, we did not find a significant correlation between the evidence of obliterative otosclerosis at preoperative CT and the results after implantation.
Conclusions
The current surgical options for AO include stapes surgery and CI. Unfortunately, to date, there are no universally accepted guidelines to determine the most suitable option for each patient, and a universally recognised definition of this condition is also lacking, making it difficult to compare the results across different studies in the literature. The surgical choice should be guided not only by the patient’s audiological profile and the presence and extent of the air-bone gap, but also by the level of speech discrimination, imaging results, and, secondarily, by the patient’s age, economic factors, hearing in the contralateral ear, and preference after thorough counselling. Both procedures present specific advantages and issues. Stapes surgery yields more variable and less predictable results and reportedly carries a higher rate of side effects. On the other hand, CI generally provides satisfactory outcomes, in most studies not significantly different from those of adult CI recipients with other aetiologies, but it is a more complex and expensive procedure and can present surgical and postoperative issues that may be challenging for both surgeons and the CI team. These challenges can include partial or incorrect insertion of the electrode array and the possibility of intraoperative gusher. Postoperatively, electrical FNS is a significant concern, potentially affecting outcomes, which must be managed by an experienced team; additionally, mapping difficulties can arise, and there is ongoing debate about the potential for progressive deterioration of results. All these aspects must be thoroughly discussed with the patient in a detailed preoperative counselling. In conclusion, the decision between stapedoplasty and CI must be personalised and well-considered, taking into account the individual characteristics of the patient and the potential risks and benefits of each option. Further comparative studies and detailed guidelines are desirable to provide clearer indications and support clinicians in therapeutic decision-making.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
SB, FF, LB: conceived the initial idea for the narrative review and developed the structure of the article; LDG, SC, DB, FL: performed the literature review and critically analyzed the sources. All authors contributed significantly to drafting the manuscript, revising it for important intellectual content, and approving the final version to be submitted. Each author has read and agreed to the published version of the manuscript.
Ethical consideration
Not applicable.
History
Received: January 7, 2025
Accepted: April 7, 2025
Figures and tables
Figure 1. The boxplot shows words recognition scores, both in quiet and with background noise, before and after cochlear implantation in the study and control groups. Circles define outliers, while an asterisk marks a large outlier.
| Study group | Control group | p value | |
|---|---|---|---|
| N | 31 (33 CI) | 31 (32 CI) | |
| F/M ratio | 18/13 | 19/12 | 0.739136 |
| Age (years) | 65.3 (range, 39-79) | 65.1 (range, 39-79) | 0.915887 |
| Unilateral/bilateral CI | 29/2 | 30/1 | 0.711332 |
| Bimodal users | 10/29 | 10/30 | 0.244659 |
| Follow-up (years) | 8.5 (range, 1-24) | 6.3 (range, 1-17) | 0.058833 |
| Preop WRS in quiet | 30.6% (range, 0-100%) | 23.7% (range, 0-65%) | 0.004355* |
| Preop WRS with background noise | 11.7% (range, 0-70%) | 6.6% (range, 0-35%) | 0.133715 |
| Complications | 5/33 (15%) | 0/32 (0%) | 0.0531 |
| Postoperative WRS in quiet | 69.4% (range, 30-100%) | 77.7% (range, 50-100%) | 0.161134 |
| Postoperative WRS with background noise | 45.7% (range, 0-95%) | 42.5% (range, 0-85%) | 0.664712 |
| WRS: words recognition score; * indicates statistically significant difference. | |||
References
- Claussen A, Gantz B. Cochlear implantation in advanced otosclerosis: pitfalls and successes. Curr Otorhinolaryngol Rep. 2022;10:49-57. doi:https://doi.org/10.1007/s40136-021-00383-1
- House H, Sheehy J. Stapes surgery: selection of the patient. Ann Otol Rhinol Laryngol. 1961;70:1062-1068. doi:https://doi.org/10.1177/000348946107000411
- Iurato S, Ettorre G, Onofri M. Very far-advanced otosclerosis. Am J Otol. 1992;13:482-487.
- Lachance S, Bussières R, Côté M. Stapes surgery in profound hearing loss due to otosclerosis. Otol Neurotol. 2012;33:721-723. doi:https://doi.org/10.1097/MAO.0b013e3182565a0e
- Merkus P, van Loon M, Smit C. Decision making in advanced otosclerosis: an evidence-based strategy. Laryngoscope. 2011;121:1935-1941. doi:https://doi.org/10.1002/lary.21904
- Berrettini S, Burdo S, Forli F. Far advanced otosclerosis: stapes surgery or cochlear implantation?. J Otolaryngol. 2004;33:165-171. doi:https://doi.org/10.2310/7070.2004.03006
- van Loon M, Merkus P, Smit C. Stapedotomy in cochlear implant candidates with far advanced otosclerosis: a systematic review of the literature and meta-analysis. Otol Neurotol. 2014;35:1707-1714. doi:https://doi.org/10.1097/MAO.0000000000000637
- Luca M, Massimilla E, Americo M. Stapes surgery in far-advanced otosclerosis. Ear Nose Throat J. 2023;102:611-615. doi:https://doi.org/10.1177/01455613211013093
- Teaima A, Elnashar A, Hakim E. Comparison of the efficacy of cochlear implantation and stapes surgery in far advanced otosclerosis: a meta-analysis study. Eur Arch Otorhinolaryngol. 2023;280:77-88. doi:https://doi.org/10.1007/s00405-022-07449-w
- Kondo M, Vasan K, Jufas N. Cochlear implantation in far advanced otosclerosis: a systematic review and meta-analysis. Laryngoscope. 2023;133:1288-1296. doi:https://doi.org/10.1002/lary.30386
- Lam C, Cornwall H, Chaudhry A. Cochlear implant outcomes in patients with otosclerosis: a systematic review. Otol Neurotol. 2022;43:734-741. doi:https://doi.org/10.1097/MAO.0000000000003574
- Assiri M, Khurayzi T, Alshalan A. Cochlear implantation among patients with otosclerosis: a systematic review of clinical characteristics and outcomes. Eur Arch Otorhinolaryngol. 2022;279:3327-3339. doi:https://doi.org/10.1007/s00405-021-07036-5
- Protocollo Comune Per La Valutazione Dei Risultati in Audiologia Riabilitativa. I Care; 1997.
- Calvino M, Sánchez-Cuadrado I, Gavilán J. Cochlear implant users with otosclerosis: are hearing and quality of life outcomes worse than in cochlear implant users without otosclerosis?. Audiol Neurotol. 2018;23:345-355. doi:https://doi.org/10.1159/000496191
- Wong D, Copson B, Gerard J. Cochlear implantation in advanced otosclerosis: utility of pre-operative radiological assessment in predicting intra-operative difficulty and final electrode position. J Laryngol Otol. 2023;137:1248-1255. doi:https://doi.org/10.1017/S0022215123000609
- Çatli T, Tokat T, Başaran Bozkurt E. Surgical considerations and audiological results of cochlear implantation in patients with otosclerosis. Turk J Med Sci. 2020;50:855-859. doi:https://doi.org/10.3906/sag-1912-238
- Lee J, Nadol J, Eddington D. Factors associated with incomplete insertion of electrodes in cochlear implant surgery: a histopathologic study. Audiol Neurotol. 2011;16:69-81. doi:https://doi.org/10.1159/000316445
- Berrettini S, Forli F, Neri E. Scala vestibuli cochlear implantation in patients with partially ossified cochleas. J Laryngol Otol. 2002;116:946-950. doi:https://doi.org/10.1258/00222150260369516
- Kabbara B, Gauche C, Calmels M. Decisive criteria between stapedotomy and cochlear implantation in patients with far advanced otosclerosis. Otol Neurotol. 2015;36:E73-E78. doi:https://doi.org/10.1097/MAO.0000000000000692
- O’Connell B, Hunter J, Wanna G. The importance of electrode location in cochlear implantation. Laryngoscope Investig Otolaryngol. 2016;1:169-174. doi:https://doi.org/10.1002/lio2.42
- Mosnier I, Bouccara D, Ambert-Dahan E. Cochlear implantation and far-advanced otosclerosis. Adv Otorhinolaryngol. 2007;65:323-327. doi:https://doi.org/10.1159/000098854
- Matterson A, O’Leary S, Pinder D. Otosclerosis: selection of ear for cochlear implantation. Otol Neurotol. 2007;28:438-446. doi:https://doi.org/10.1097/MAO.0b013e31803115eb
- Atanasova-Koch S, Issing P. Cochlear implantation outcomes in patients with otosclerosis: a single-centre study. Eur Arch Otorhinolaryngol. 2022;279:3929-3936. doi:https://doi.org/10.1007/s00405-021-07157-x
- Schvartz-Leyzac K, Zwolan T, Pfingst B. Effects of electrode deactivation on speech recognition in multichannel cochlear implant recipients. Cochlear Implants Int. 2017;18:324-334. doi:https://doi.org/10.1080/14670100.2017.1359457
- Fishman K, Shannon R, Slattery W. Speech recognition as a function of the number of electrodes used in the SPEAK cochlear implant speech processor. J Speech Lang Hear Res. 1997;40:1201-1215. doi:https://doi.org/10.1044/jslhr.4005.1201
- Burmeister J, Rathgeb S, Herzog J. Cochlear implantation in patients with otosclerosis of the otic capsule. Am J Otolaryngol. 2017;38:556-559. doi:https://doi.org/10.1016/j.amjoto.2017.05.011
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 931 times
- PDF downloaded - 141 times



