Rhinology
Vol. 45: Issue 3 - June 2025
Ostiomeatal complex preservation: submucosal inferior meatal antrostomy for maxillary sinus pathologies
Abstract
Objective. Endoscopic inferior meatal antrostomy (EIMA) is feasible for treating maxillary sinus pathologies. We describe submucosal inferior meatal antrostomy (SIMA), a new ostiomeatal complex (OMC) sparing technique based on EIMA.
Materials and methods. Medical records of patients who underwent SIMA for maxillary sinus pathologies were retrospectively reviewed. Data collected included age, gender, presenting symptoms, preoperative and postoperative endoscopic and computed tomography findings, early followup duration, and complications.
Results. Twenty-two operated maxillary sinuses, in 20 patients, were included. Pathologies included displaced dental implant (n = 4), odontogenic sinusitis (n = 6), retention cyst (n = 5), antrochoanal polyp (n = 5) and fungus ball (n = 2). SIMA provided excellent access and view, and the OMC and the inferior meatus mucosa remained intact. Nineteen patients were completely cured following a rapid recovery and needed no further intervention. No intra-operative or postoperative complications occurred, and recirculation was not observed. One case failed due to a persistent odontogenic infection.
Conclusions. SIMA provides an improved access and view when treating non-OMC-dependent maxillary sinus pathologies, while maintaining the integrity of the middle and inferior meatuses mucosa.
Introduction
Pathologies of the maxillary sinus, that are not caused by ostiomeatal complex (OMC) obstruction, are not rare. Among others, they include retention cysts, antrochoanal polyps, fungus balls, odontogenic infections, migrating dental implants and ectopic teeth. Such cases are usually treated by functional endoscopic sinus surgery (FESS), during which an endoscopic middle meatal antrostomy (EMMA) is performed, often together with ethmoidectomy of the anterior and other adjacent sinuses. Traditionally, the purpose of EMMA is to open the obstructed natural ostium of the maxillary sinus, allowing improved drainage and ventilation of the sinus and the OMC. The OMC represents the final common pathway for drainage and ventilation of the frontal, maxillary, and anterior ethmoid air cells. When it is obstructed or narrowed, sinusitis may develop in these sinuses 1,2.
Therefore, EMMA is appropriate to treat maxillary sinus pathologies secondary to OMC obstruction. However, when the pathology arises primarily from the maxillary sinus cavity, dissecting the OMC is questionable. Any surgical intervention in a normal middle meatus may cause postoperative complications, especially middle meatal adhesions, which might disrupt the integrity of the OMC and lead to subsequent sinusitis 3-5.
In previous studies we have discussed the rationale for using endoscopic inferior meatal antrostomy (EIMA) to treat a variety of pathologies arising from the maxillary sinus. We have shown that this technique enables excellent access to anteroinferior lesions and the preservation of OMC integrity 6,7.
Herein, we present a novel technique for OMC preservation when treating the same maxillary sinus pathologies, using submucosal inferior meatal antrostomy (SIMA). This technique is based on the same concept as that used for EIMA, but also allows preservation of inferior meatus integrity.
Materials and methods
Inclusion criteria
Patients who had maxillary sinus pathology, which arises from the sinus cavity and not secondary to OMC obstruction, were included. Those with benign or malignant tumours were excluded.
Setting and patients
Medical records of patients who underwent SIMA at A.R.M. Assuta Medical Center (Tel-Aviv, Israel) between June 2021 and September 2022 were retrospectively reviewed. Data collected included age, gender, presenting symptoms, side involved, preoperative computed tomography (CT) findings, postoperative CT (if required), surgical approach, early follow-up duration, postoperative findings and complications. Demographic, clinical and imaging characteristics are presented in Table I.
SIMA surgical technique
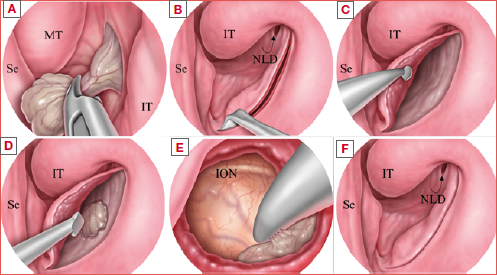
Following induction of general anaesthesia, a 0.5-3-inch neuropatty soaked in 1:1000 adrenalin was inserted lateral to the inferior turbinate. After medialisation of the inferior turbinate, the lateral nasal wall was inspected, and the nasolacrimal duct opening (Hasner’s valve) was detected. A bent 22-gauge spinal needle was used for submucosal hydrodissection of the nasal floor and inferior meatal wall. Then, using an ophthalmic angled crescent knife (Surgistar Inc., Vista, CA, USA) or an angled microdissection diathermia needle, an incision was made in the coronal plane, starting anterior to Hasner’s valve and right posterior to the inferior turbinate head, continuing vertically on the lateral nasal wall and horizontally on the nasal floor until the nasal septum. To create a well sized flap, it is important to make the nasal floor cut as anterior as possible, but still posterior to the piriform aperture. Using a curved suction-freer and an otologic curved round knife, a submucosal inferior meatal dissection was gently performed, bordered medially by the septum, anteriorly by the inferior turbinate head and piriform aperture, posteriorly by the posterior insertion of the inferior turbinate, and superiorly by the horizontal attachment of the inferior turbinate. The inferior medial maxillary wall was penetrated at its thinner posterior portion using a Cottle elevator or a 70° sinus curette. Inferior antrostomy was created using cutting forceps, a backbiter and a Kerrison rongeur as needed. The antrostomy was enlarged according to the sinus pathology nature and its location, measuring at its anterior-superior diameter approximately 1 to 3 cm. Straight and curved instruments, including curved shavers, if needed, were used to access the relevant areas. After entering the maxillary sinus, the posterior aspect was viewed with a 0° endoscope and the lateral and anterior aspects was viewed with a 45° endoscope. The lesion/pathology was detected and removed, the mucosal flap was replaced at its original position, and the inferior turbinate was relateralised. Nasal packing was not needed. The different steps of SIMA, performed to remove a tooth root with a fungus ball and an antrochoanal polyp (illustrated) are shown in the Figure 1 and Cover figure, respectively.
Statistical analysis
The data were analysed using descriptive statistics; continuous variables were summarised using mean and standard deviation and categorical variables were summarised using number and percentage.
Results
Twenty patients (13 males, 7 females) with a median age of 50 years (range, 17-74) underwent SIMA. As 2 patients had a two-sided surgery, a total of 22 maxillary sinuses were operated on. Six patients were asymptomatic (among them, 3 had dislocated dental implants and 3 had large maxillary cysts before a sinus lift), 9 reported purulent nasal discharge, and 5 suffered from unilateral nasal obstruction.
All patients underwent preoperative nasal endoscopy and CT of the paranasal sinuses (Fig. 2). The most common endoscopic finding was middle meatal discharge (10 patients). Five patients had an antrochoanal polyp, and one, who had previously undergone endoscopic sinus surgery (ESS), had a migrated dental implant observed by a flexible endoscope through a middle antrostomy. Four patients had a normal endoscopic examination.
A preoperative paranasal sinuses CT scan revealed a non-OMC-dependent maxillary sinus abnormality in all patients, including odontogenic maxillary sinusitis (6 patients), large maxillary retention cyst (5 patients), migrated dental implants (4 patients), antrochoanal polyp (5 patients), fungus ball (one patient), and a tooth root surrounded by a fungus ball (one patient).
All patients underwent SIMA alone to treat their primary maxillary sinus pathology, except for the patient with the migrated dental implant, who also underwent EMMA since the dental implant was not detected. However, even following EMMA and subsequent intraoperative skull X-ray imaging, no implant was found. No complications occurred during surgery.
The postoperative follow-up period ranged from 6 to 18 months (median, 10 months). No postoperative complications occured. Nineteen of 20 patients recovered quickly; they were asymptomatic, and endoscopic examination showed a normal anatomy, i.e., both the inferior and middle meatuses were fully intact (Fig. 3). A single patient, who had odontogenic sinusitis, did not improve after surgery and was referred to his dentist for further dental intervention. Occasionally, for dental indications, a postoperative CT (usually cone-beam CT) was performed to examine the maxillary sinus cavity prior to a sinus lift procedure.
Discussion
FESS aims to preserve the normal mucosa of the nose and paranasal sinuses as much as possible. Stammberger et al. have shown that when treating chronic maxillary sinusitis, the sinus becomes healed after opening the sinus outflow tract 1. We have previously shown that non-OMC-dependent pathologies of the maxillary sinus can be accessed by an EIMA instead of an EMMA. This technique targeted 2 main principles: 1. preservation of the uninvolved OMC, and 2. easier access to lesions located anteroinferiorly to the maxillary sinus cavity. Recovery following EIMA was excellent and fast with minimal symptoms 6,7.
The SIMA technique, used in the current study, maintains the same principles. However, unlike the previously described EIMA, we did not leave a permanent opening (antrostomy) in the inferior medial maxillary sinus wall. Instead, the maxillary sinus cavity was entered submucosally to remove the lesion. The anterior mucosal incision facilitates the widening of the antrostomy anteriorly as much as required. Hasner’s valve is located just below the level of the inferior turbinate insertion, at least 1 cm above the nasal floor, and therefore remains unharmed above the antrostomy. None of the patients experienced any complication related to the nasolacrimal duct system. A postoperative endoscopic examination revealed an intact nasal mucosa and anatomy, and no remnant inferior meatal antrostomy was observed.
Due to the mucosal flap used to restore the maxillary sinus wall, SIMA has several advantages compared to EIMA: it prevents potential mucus recirculation, avoids inferior meatal adhesions, and preserves both the anterior and the medial maxillary walls for a future potential sinus lift. Lastly, since the mucosal flap provides complete restoration of the inferior meatus, the size of the antrostomy is not a concern and can be enlarged up to 3 cm.
SIMA is superior to the OMC-preservative prelacrimal recess approach (PLRA) in 2 instances: first, the PRLA is not suitable for 31.5% of patients who have type I lacrimal recess, where the distance between the nasolacrimal duct and the anterior maxillary wall is less than 3 mm. Second, unlike SIMA, PLRA often requires anterior maxillary wall bony removal – either by a chisel or a drill – and temporary nasolacrimal duct dislocation from its bony canal 8-10. Leaving both the anterior nasal aperture and the anterior maxillary wall untouched when doing SIMA avoids injury to the anterior superior alveolar nerve and subsequent neurosensory sequelae such as dental para-aesthesia and upper lip numbness 11. None of these symptoms were reported after SIMA.
SIMA can be performed even when the OMC is inflamed secondary to maxillary sinus primary pathology. The OMC is expected to heal following eradication of the maxillary sinus pathology. However, when the ethmoid or even the frontal sinus are also heavily involved, EMMA is preferred.
Based on our study and ongoing experience, SIMA is recommended for the following maxillary sinus primary pathologies: antrochoanal polyp, large retention cyst, fungus ball, migrated dental implants and non-active odontogenic disease. The authors do not recommend SIMA for active odontogenic infection, like oroantral fistula or infected tooth, unless it is simultaneously performed with the elimination of the dental source of infection.
SIMA has 2 potential limitations. The first is the learning curve required to become familiar with the unconventional working angle in the inferior meatus; nevertheless, this learning curve is relatively short. The second limitation is the absence of an opened antrostomy which prevents evaluating the sinus cavity endoscopically during the follow-up period. However, in most cases presented herein, it was sufficient to rely on the patient’s symptoms and endoscopic examination during follow-up. For instance, following antrochoanal polyp, removal is easily evaluated by inserting a thin fibrescope through the accessory ostium. If disease recurrence is suspected, we recommend performing a minimal radiation cone-beam CT.
Currently, the authors use SIMA routinely for the above-mentioned indications. However, a prospective and longer follow-up are ongoing to strengthen the rationale for this approach.
Conclusions
EMMA remains the standard approach for maxillary sinus disease that is secondary to OMC incompetence. SIMA is simple, minimally invasive and OMC preservative technique, which is adequate for treating most maxillary pathologies that are not related to OMC obstruction, including antrochoanal polyp, retention cyst, fungus ball, migrated dental implants and non-active odontogenic sinusitis.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
RL, MM: conception and design of the study, acquisition of the data, analysis and interpretation of the data; drafted the article and revised it for important intellectual content; gave final approval of the version to be submitted; agree to be accountable for all aspects of the work; SS: analysis and interpretation of the data; drafted the article and revised it for important intellectual content; gave final approval of the version to be submitted; agree to be accountable for all aspects of the work. RL, MM equally contributed to this work.
Ethical consideration
This study was approved by Assuta Medical Center’s institutional ethics committee (Approval number: ASMC-0069-21, year 2022). The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Informed consent was obtained from patients at the time of original data collection.
The data were anonymously collected and analyzed.
History
Received: February 16, 2024
Accepted: November 16, 2024
Figures and tables
Figure 1. The SIMA technique for tooth root removal (A) Mucosal incision at the lateral nasal wall, 1-2 mm posterior to the skin-mucosa junction, along the level of the inferior turbinate and down to the nasal floor. Note the septum on the left; (B) The mucosal flap is elevated posteriorly to create a “pouch” between the mucosal flap and (C) the bony medial maxillary wall; (D) The inferior meatal antrostomy is then created and widened; (E) The tooth root is released throughout the antrostomy; (F) The mucosal flap is returned to its previous position. Se: septum; IM; inferior meatus; IT: inferior turbinate; NF: nasal floor; MMW; medial maxillary wall; F: flap; IMA: inferior meatal antrostomy.
Figure 2. Preoperative and postoperative CT scan of the paranasal sinuses. (A) A preoperative scan showing bilateral opacification with a dense opaque lesion in the left maxillary sinus (tooth root) surrounded by a less condensed hallow (fungus ball); (B) Four months after EMMA and SIMA for the right and left maxillary sinuses, respectively. Note the intact anatomy of the left maxillary sinus and the untouched ostiomeatal complex.
Figure 3. SIMA 4-month postoperative endoscopic evaluation. (A) Normal untouched middle meatal structures; (B) Normal-looking inferior meatus. The inferior antrostomy is fully covered with a well-healed mucosal flap. BE: bulla ethmoidalis; IM: inferior meatus; IT: inferior turbinate; MM: middle meatus; MT: middle turbinate; UP: uncinate process.
| Patient | Gender | Age | Side | Presenting symptoms | Endoscopic findings | Preoperative CT | Diagnosis | Follow- up (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 55 | L | Nasal discharge | Purulent middle meatal discharge | Full maxillary sinus opacification, OAF, bone sequester | Odontogenic sinusitis | 11 |
| 2 | M | 50 | R | Nasal discharge, teeth pain | Purulent middle meatal discharge | Full maxillary sinus opacification, periapical cyst | Odontogenic sinusitis | 9 |
| 3 | F | 47 | L | Nasal discharge | Purulent middle meatal discharge | OAF | Odontogenic sinusitis | 8 |
| 4 | M | 68 | L | None (before sinus lift) | None | Rounded opacification | Maxillary retention cyst | 10 |
| 5 | M | 52 | L | Nasal discharge | Right purulent middle meatal discharge | Rounded opacification | Maxillary retention cyst | 10 |
| R | Periapical cyst+ full maxillary sinus opacification | Odontogenic sinusitis | ||||||
| 6 | M | 39 | L | Nasal obstruction | Intranasal polyp | Maxillary sinus and nasal cavity opacification | Antrochoanal polyp | 16 |
| 7 | M | 64 | L | Nasal discharge | Purulent middle meatal discharge | Opaque foreign body surrounded by a less dense halo | Tooth root + fungus ball | 9 |
| 8 | M | 44 | R | None | Story of previous FESS and migrated dental implant in maxillary sinus | Opaque foreign body | Migrated dental implant | 14 |
| 9 | F | 46 | R | None (prior to sinus lift) | None | Rounded opacification | Retention cyst | 12 |
| 10 | M | 53 | L | None | Purulent middle meatal discharge | Opaque foreign body | Migrated dental implant | 18 |
| 11 | M | 69 | L | None | None | Opaque foreign body | Migrated dental implant | 10 |
| 12 | F | 59 | R | Nasal discharge | Purulent middle meatal discharge | Opaque foreign body + full maxillary sinus opacification | Migrated dental implant | 8 |
| L | Retention cyst | |||||||
| 13 | M | 51 | R | Nasal obstruction | Intranasal polyp | Maxillary sinus and nasal cavity opacification | Antrochoanal polyp | 11 |
| 14 | M | 28 | R | Nasal obstruction | Intranasal polyp | Maxillary sinus and nasal cavity opacification | Antrochoanal polyp | 11 |
| 15 | F | 50 | R | Nasal discharge | Purulent middle meatal discharge | Full maxillary sinus opacification | Fungus ball | 14 |
| 16 | M | 17 | L | Nasal obstruction | Intranasal polyp | Maxillary sinus and nasal cavity opacification | Antrochoanal polyp | 9 |
| 17 | M | 42 | R | Nasal obstruction | Intranasal polyp | Maxillary sinus and nasal cavity opacification | Antrochoanal polyp | 10 |
| 18 | F | 48 | L | None (before sinus lift) | None | Rounded opacification | Retention cyst | 13 |
| 19 | F | 62 | L | Nasal discharge | Purulent middle meatal discharge | Maxillary sinus opacification, OAF | Odontogenic sinusitis | 10 |
| 20 | M | 57 | L | Nasal discharge | Purulent middle meatal discharge | Maxillary sinus opacification, OAF | Odontogenic sinusitis | 9 |
| M: male; F: female; R: right; L: left; OAF: oroantral fistula; FESS: functional endoscopic sinus surgery. | ||||||||
References
- Stammberger H, Hawke M. Essentials of Endoscopic Sinus Surgery. Mosby; 1993.
- Schaefer S, Li J, Chan E. Combined anterior-to-posterior and posterior-to-anterior approach to paranasal sinus surgery: an update. Laryngoscope. 2006;116:509-513. doi:https://doi.org/10.1097/01.Mlg.0000205615.46937.94
- May M, Levine H, Mester S. Complications of endoscopic sinus surgery: analysis of 2108 patients – incidence and prevention. Laryngoscope. 1994;104:1080-1083. doi:https://doi.org/10.1288/00005537-199409000-00006
- Ramadan H. Surgical causes of failure in endoscopic sinus surgery. Laryngoscope. 1999;109:27-29. doi:https://doi.org/10.1097/00005537-199901000-00006
- Musy P, Kountakis S. Anatomic findings in patients undergoing revision endoscopic sinus surgery. Am J Otolaryngol. 2004;25:418-422. doi:https://doi.org/10.1016/j.amjoto.2004.06.002
- Landsberg R, Warman M, Margulis A. The rationale for endoscopic inferior meatal antrostomy. ORL J Otorhinolaryngol Relat Spec. 2019;81:41-47. doi:https://doi.org/10.1159/000496087
- Landsberg R, Masalha M, Margulis A. Endoscopic inferior meatal antrostomy for antrochoanal polyps: a long-term follow-up. ORL J Otorhinolaryngol Relat Spec. 2022;84:336-341. doi:https://doi.org/10.1159/000518279
- Morrissey D, Wormald P, Psaltis A. Prelacrimal approach to the maxillary sinus. Int Forum Allergy Rhinol. 2016;6:214-218. doi:https://doi.org/10.1002/alr.21640
- Simmen D, Veerasigamani N, Briner H. Anterior maxillary wall and lacrimal duct relationship – CT analysis for prelacrimal access to the maxillary sinus. Rhinology. 2017;55:170-174. doi:https://doi.org/10.4193/Rhino16.318
- Zhou B, Huang Q, Sun J. Resection of inverted papilloma of the maxillary sinus via a prelacrimal recess approach: a multicenter retrospective analysis of surgical efficacy. Am J Rhinol Allergy. 2018;32:518-525. doi:https://doi.org/10.1177/1945892418801243
- Machado A, Briner H, Schuknecht B. Assessment of the anterior superior alveolar nerve and its impact on surgery of the lateral nasal wall. Rhinology. 2021;59:475-480. doi:https://doi.org/10.4193/Rhin21.223
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1115 times
- PDF downloaded - 201 times



