Audiology
Vol. 45: Issue 3 - June 2025
Italian adaptation of Listening Effort Assessment Scale and Fatigue Assessment Scale questionnaires
Abstract
Objective. The purpose of this study is to adapt linguistically and culturally the Listening Effort Assessment Scale (EAS) and Fatigue Assessment Scale (FAS) questionnaires into Italian (EAS-IT and FAS-IT) and to investigate the reliability and validity of these scales in normal hearing and hearing-impaired subjects.
Methods. The Italian adaptation of the EAS and FAS questionnaires was conducted based on back and forward translation methodology. Both questionnaires were administered to 101 normal hearing (NH) subjects and 88 hearing-impaired subjects including 19 hearing aid users (HA), 50 cochlear implant users (CI) and 19 affected by single-sided deafness (SSD).
Results. Both questionnaires showed a high reliability (Cronbach’s α was 0.953 for EAS-IT and 0.837 for FAS-IT). EAS-IT showed high internal consistency with item-rest correlations. The interitem correlation of the FAS-IT shows a difference in the internal consistency of item 4. A high significance between the NH group and the 3 hearing loss groups (HA, CI, SSD) was found for EAS-IT, but no significant difference was found between NH and the single hearing-impaired groups for FAS-IT.
Conclusions. EAS-IT showed good internal reliability and validity and is sensitive to hearing loss.
Introduction
The restoration of auditory function for individuals experiencing hearing loss is feasible in the majority of cases in contemporary settings. Today, different types of hearing devices are available depending on the degree and typology of hearing loss. It is possible to choose between conventional hearing aids in case of sensorineural hearing loss, cochlear implant in profound deafness, or implantable hearing devices in case of mixed or conductive hearing loss. However, comfortable hearing is not always achieved simply by wearing an electronic hearing device; in fact, hearing differs from person to person because several factors play a key role in this sensory ability 1-2.
These include, among others, age at onset of hearing loss 3, time of deprivation, aetiology, time of device use, associated disabilities, and memory and cognitive capacities. In some case, patients affected by similar degrees of hearing loss and speech perception ability may exhibit different performances and different quality of life outcomes.
The greatest difficulty reported by patients is listening in adverse situations like in noise or in reverberant spaces where a great deal of energy must be expended to understand the sound message. They report headaches, frontal heaviness, fatigue and tiredness at the end of the day. Such energy expenditure is called listening effort 4-5. Measuring just the magnitude of hearing loss is therefore insufficient for a comprehensive assessment of hearing ability. In order to understand the global auditory capacities, it is essential to evaluate the multiple domains involved. In particular, it is important to investigate listening effort and fatigue domains 6.
A “gold standard” procedure to evaluate listening effort does not exist as different aspects are involved in this domain. Three test typologies are currently used: cognitive-behavioural (e.g. dual-task paradigm), physiological (EEG or pupillometry measures), and self-report tests 6.
For practical reasons, subjective questionnaires are often used because of the simplicity of administration and their repeatability. To date, there are only a few specific questionnaires in the literature to evaluate listening effort in subjects with hearing loss. In most studies the Speech, Spatial, and Qualities (SSQ) Hearing Scale questionnaire is used7. In this questionnaire, only 3 of 49 items refer directly to listening effort: “Do you have to concentrate very much when listening to someone or something?” (item 14 - Qualities subscale); “Do you have to put in a lot of effort to hear what is being said in conversation with others?” (item 15 - Qualities subscale) and “Can you easily ignore other sounds when trying to listen to something?” (item 18 - Qualities subscale).
The only patient-reported outcome measure (PROM) that is hearing-specific for evaluating listening effort is the Listening Effort Questionnaire-Cochlear Implant (LEQ-CI). This tool is targeted to adult CI recipients with profound hearing loss 8.
Recently Alhanbali and colleagues introduced 2 PROMs for adults with hearing loss of any degree and typologies: the Listening Effort Assessment Scale (EAS) and the Fatigue Assessment Scale (FAS) 9.
The EAS is a self-administered 6-item questionnaire that measures effort in different conditions: listening in the presence of different speakers, in a noisy environment, listening to music, etc. The patient is required to respond to each item using a visual analogue scale (VAS), with a higher total score being associated with greater effort 9.
The FAS is also a self-administered questionnaire that was taken from an earlier study by Michielsen et al. 10. It consists of 10 items that explore different aspects of fatigue and has been widely used in a variety of conditions. The response to each item is rated on a VAS scale.
The 2 questionnaires have good psychometric properties, take a short time to complete and assess fatigue and listening effort in realistic situations. Both the EAS and FAS questionnaires are in English and have been translated and validated in several languages, but not in Italian 11,12.
The purpose of this study is to linguistically and culturally adapt both the EAS and FAS questionnaires into Italian (EAS-IT and FAS-IT) and to investigate the reliability and validity of these scales in normal hearing and hearing-impaired subjects.
Materials and methods
Fatigue Assessment Scale (FAS) questionnaire
The FAS is a self-administered questionnaire described and validated by Michielsen et al. 10. It consists of 10 items assessing different types of fatigue (physical, cognitive and mental). The patient is asked to answer each item on a visual analogue scale from 1 to 5, where 1 corresponds to never and 5 to always. A higher total score correlates with a higher degree of fatigue.
The validation study showed high reliability, validity and internal consistency. The population with hearing loss has a higher average score compared to subjects with normal hearing, but no differences were reported between different types of hearing loss 9.
Listening Effort Assessment Scale (EAS) questionnaire
The EAS questionnaire was first described and validated in 2017 by Alhanbali et al. 9.
It is a self-administered scale, with 3 of the items taken from the SSQ hearing scale 4 and the other 3 were extracted from a doctoral dissertation.
The items explore listening effort in different situations. The patient is asked to respond to each item on a VAS ranging from 0 to 10, where 0 corresponds to no effort and 10 corresponds to a lot of effort. A higher total score corresponds to a greater degree of listening effort.
In the study of Alhanbali et al. a significant statistical correlation between hearing-impaired (with higher score) and normal hearing subjects was reported 9.
Cross-cultural adaptation of the EAS-IT and the FAS-IT
The Italian adaptation of the EAS and FAS questionnaires was carried out according to the guide proposed by Hall et al. 13.
The process is based on back and forward translation methodology and consists of 6 steps: (a) obtaining permission from the corresponding authors of the studies responsible for developing the original EAS and FAS questionnaires; (b) forward translation of the 2 questionnaires into Italian, performed independently by 2 native speakers (audiologist and otolaryngologist); (c) committee review: a working group not involved in the previous stage reviewed and incorporated all comments and changes; (d) back-translation into English by a native English speaker with knowledge of Italian to check for consistency with the English version; (e) comparison of the 2 English versions (original and translated from Italian) by the original authors and analysis to highlight any substantial differences; (f) field testing: both the questionnaires were administered to 100 normal hearing subjects. Both questionnaires were then administered to a sample of hearing-impaired subjects.
Sample size
Based on previous validated and translated versions and statistical sampling power, a sample size of at least 101 normal hearing (NH) and 88 hearing-impaired subjects was estimated as necessary for both the EAS and FAS adaptations.
The sample size was considered sufficiently large because both the EAS and FAS scales are relatively short (6 and 10 items, respectively): the subject-to-item ratio is over 30 in the case of the EAS and close to 19 in the case of the FAS, which is above the average of similar studies 14. In addition, both scale measures are unidimensional, i.e., they measure a single latent structure so that the sample size is in line with the recommendation in the literature 15.
Finally, the group-specific sample sizes were set to ensure the 0.05 significance of a one-way ANOVA test (or Kruskal-Wallis in the case of non-normality), which has been used in the assessment of discriminant validity to compare normal hearing individuals with different groups of hearing-impaired individuals. These sample size determinations, based on a significance level of 0.05, an effect size of 0.4 and power of 0.8, were obtained using the pwr R package 16.
Participants
In all, 189 subjects (75 males) aged 18-81 years with and without hearing loss participated in the study (Tab. I). Participants were recruited at the ENT outpatient facilities of the “Guglielmo da Saliceto” Hospital in Piacenza, Italy.
The inclusion criteria encompassed individuals of both genders, aged over 18 years, of Italian mother tongue, able to consent to the study and with a recent pure-tone audiogram (< 3 months).
Subjects with cognitive impairment or any other morbidity that might prevent them from understanding and answering the self-administered questionnaires were excluded. All subjects signed the informed consent form before the questionnaires were administered.
Patients enrolled in the study were divided into 4 groups according to pure tone threshold average (PTA) at 500, 1000, 2000, 4000 Hz frequencies and type of hearing device used. The groups were: (1) Normal Hearing (NH): subjects with bilateral PTA less than 30 dB HL; (2) Hearing Aids (HA): subjects using bilateral hearing aids with an unaided PTA between 35 and 90 dB HL; (3) Cochlear Implant (CI): subjects using unilateral CI with unaided PTA greater than 90 dB HL at the side of the CI; (4) Single-Side Deafness (SSD): subjects not using any device, with PTA less than 30 dB HL in the better ear and greater than 70 dB HL in the worse ear. All participants in the CI and HA groups had used their hearing devices for at least 6 months.
Patients in the CI group were implanted on the side with the worse hearing threshold (profound hearing loss). Specifically, 30 subjects were implanted on the right side and 20 on the left. Hearing threshold on the contralateral side ranged from moderate to profound degree. Only 5 patients had a moderate HL (PTA between 50 and 70 dB HL), but all had a ski-slope threshold configuration with moderate threshold at low frequencies and profound threshold at high frequencies. None of the patients in the CI group used a device on the better hearing ear.
All subjects in the SSD group had been affected by unilateral profound hearing loss for at least one year: 7 on the right and 19 on the left side. The aetiologies were 12 sudden hearing loss, 3 unknown, one head trauma, one meningitis, one congenital deafness and one neuroma of the 8th cranial nerve.
Statistical analysis
Statistical analysis was carried out in order to identify the basic dimensions of validity. Cronbach’s α was calculated to measure the internal consistency of the scale, which provides information about the ability of the scale to accurately assess single construct. Cronbach’s α is a number between 0 and 1, with the recommended value of item-total correlation being 0.30 and above 17. In particular, values < 0.4 correspond to low reliability, values between 0.4 and 0.6 to uncertain reliability, values between 0.6 and 0.8 to acceptable reliability and values > 0.8 to good reliability.
Item reliability was examined by calculating the corrected item-total correlation to assess the extent to which an individual item contributes to the total score of the scale. It is calculated as the Pearson correlation between the scores of an individual item and the total score obtained by summing all the remaining items. Item reliability was guaranteed if the item correlates significantly with the total score. In addition, Cronbach’s alpha was recalculated by dropping each item in turn to assess whether the removal of an item had a significant impact on the index. Removals that increase the index are associated with potentially problematic items.
To assess the discriminant validity of the scales, we compared the scores of the normal hearing subjects with those of the different groups of hearing-impaired patients. The test used to compare group medians is Kruskal-Wallis (one-way ANOVA was rejected due to the failure of the normality assumptions for both the EAS and the FAS scales). Post-hoc analysis was performed using Dunn’s test, which consistently with Kruskal-Wallis, does not require normality. Spearman rank correlation was used to assess the relationship between EAS and FAS scores in the overall sample and within groups. The same tool was applied to study the relationship between scores and age. To compare the medians of the scores between genders (within groups), a non-parametric Wilcoxon test was used.
Results
The final versions of the FAS-IT and EAS-IT can be found in Appendices 1 and 2.
Factor analysis EAS-IT
RELIABILITY
Cronbach’s α for the total score of the EAS-IT was 0.953. The scoring of the individual items also showed high internal consistency with item-rest correlations ranging from 0.757 (item 3) to 0.916 (item 4) and Cronbach’s α ranging from 0.937 (item 2) to 0.955 (item 3) (Tab. II).
Factor analysis FAS-IT
RELIABILITY
Cronbach’s α for the total score of the EAS-IT was 0.837. The inter-item correlation (Tab. III) and the correlation matrix (Tab. IV) showed a difference in the internal consistency of item 4 (item-rest correlation of 0.156; Cronbach’s α of 0.862). The other items have similar values (Tabs. II-IV).
Group comparisons
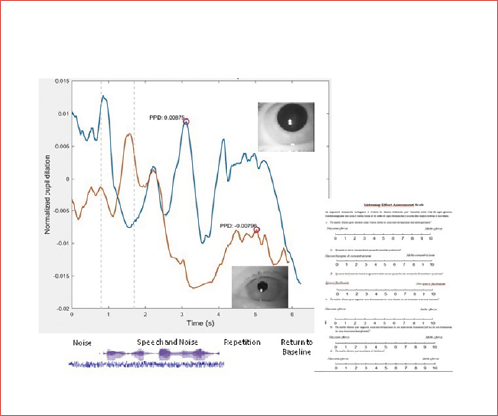
Table V shows the median, mean, standard deviation and range of scores for the EAS-IT and FAS-IT questionnaires in the 4 groups. The mean scores of the 2 questionnaires are shown in Figure 1.
Statistical analysis of the EAS-IT showed high significance between the NH group and the 3 single hearing loss groups (HA, CI, SSD) (Kruskal-Wallis chi-square equal to 93.345, df = 3, p < 2.2 e-16; Dunn’s test results equal to 0.0000). Dunn’s test showed that there was no significant correlation between CI and HA (0.3428); between SSD and CI (0.4434); and between SSD and HA (0.4137).
The inter-group comparative analyses of the FAS-IT showed similar median and mean scores between the 4 groups. No significant difference was found between NH and the single hearing-impaired groups (HA, CI, SSD) with a Kruskal-Wallis chi-square of 10.691, df = 3 and p = 0.01352.
The Dunn test confirmed the low significance between CI and HA (0.0200), between NH and CI (0.0073), and between SSD and CI (0.0023).
There were no significant differences (Spearman) between age and the EAS and FAS scores. Similarly, we did not find any statistically significant difference in the median scores between genders, as assessed by Wilcoxon tests.
EAS-IT and FAS-IT correlation
For the total sample, the Spearman correlation between the EAS-IT and FAS-IT scores was 0.20 (p = 0.0049).
Figure 2 shows the 2 scores in the 4 groups. The correlation was significant in the NH (rho = 0.46 p < 0.001) and CI (rho = 0.297, p = 0.036) groups, but not in the HA (rho = 0.24, p = 0.301) and SSD (rho =-0.17, p = 0.258) groups.
Discussion
The aim of this study was to determine the reliability and validity of the Italian adapted versions of the EAS and FAS questionnaires. Both showed good reliability, but only the EAS showed acceptable internal consistency. Reliability was assessed using Cronbach’s α. The Cronbach’s α coefficient of the Italian version of the EAS was 0.95, which is very close to the original study (0.94) 9, as well as the Arabic (0.91) 12 and Danish (0.93) 11 adaptations.
Cronbach’s α coefficient of the Italian version of the FAS was 0.84, which is very close to the original study by Michielsen et al. (0.87) 10 and to the Arabic adaptation (0.88) 12.
The correlation between the different items of the EAS-IT (0.76-0.92) showed a high internal consistency. The values were comparable to those of the original study by Alhanbali et al. 9 (0.63-0.83).
In contrast, we found a low consistency of the item 4 of the FAS-IT with the other items. In fact, item 4 “I have enough energy for the everyday life” correlated weakly with the other items. The answers to the Italian version of this item, imply that “Never” corresponds to a state of fatigue and “Always” to a state of well-being. The answers to the other items are exactly the opposite, with “Never” corresponding to a state of well-being and “Always” to a state of fatigue.
In the Arabic adaptation of the FAS, the authors found a weak correlation of another item with the others. This was item 3 “I do not do much during the day”. For this reason, the item 3 was removed from the Arabic questionnaire 9.
In the comparison between normal hearing and hearing-impaired subjects, only the EAS-IT score was able to discriminate between them; in fact, normal hearing subjects showed a significantly lower level of listening effort (in terms of overall score) compared to hearing-impaired subjects. On the other hand, no significant differences were found between normal hearing and hearing-impaired listeners when using the FAS-IT. For these reasons, the results of the EAS-IT questionnaire are predictive in the detection of hearing impairment.
Unlike us, Alhanbali et al. found a correlation between normal hearing and hearing-impaired subjects for both EAS and FAS questionnaires, both in the original study and in the Arabic adaptation 9,12.
Similar to the 2 studies by Alhanbali and the Danish EAS adaptation, our results showed that there are no differences between the 3 groups of hearing-impaired subjects (HA, CI and SSD) in both EAS-IT and FAS-IT 9-12. It is interesting to note that regardless of hearing loss type, degree and side of deafness, patients with hearing loss had similar scores, i.e. similar degree of listening effort. These data suggest that unilateral (single-sided) deafness is associated with a similar level of listening effort as bilateral deafness, such as with hearing aids or cochlear implants.
There are only a few studies in the literature that have specifically investigated the level of listening effort in patients with SSD. In particular, there is no specific research that has evaluated patients with SSD in comparison to patients with hearing aids or cochlear implants. A recent study by Mitton et al. 18 assessed the level of listening effort in patients with SSD, but in contrast to our study, the subjects were CI recipients. The authors showed that subjects with CI in SSD had similar degree of listening effort as those with bilateral hearing loss and use of unilateral or bilateral CI.
Furthermore, there is no agreement in the literature on the methodology to assess listening effort in different typologies of patients with hearing loss. To date, there are no questionnaires that are specifically designed for patients with hearing loss. In the majority of cases, the Speech Spatial Qualities (SSQ) or the general quality of life questionnaires have been used 18. Other studies have used physiological measures (such as pupillometry) to assess listening effort 19.
The differences that we found between the EAS and FAS questionnaires are due to the inherent nature of the FAS tool; in fact, it is not a symptom (hearing) specific questionnaire, but is designed to assess fatigue as a more general concept. Subjects in this study may report fatigue related to global health rather than hearing ability.
In a number of chronic health conditions, fatigue is a commonly reported experience.
For these reasons, there are several different types of fatigue. Among these, it is well know mental fatigue and physical fatigue which correspond to a reduced ability, or desire, to carry out mental or physical tasks. Another typology of fatigue is listening-related fatigue which is defined as “the extreme tiredness resulting from effortful listening” 5. Listening-related fatigue is an extreme stage of listening effort because “Listening effort” is a construction that includes the concept of effort during a listening task. In particular, effort is defined as “the deliberate allocation of mental resources to overcome obstacles in goal pursuit when carrying out a task” and listening effort as the “effort involved in carrying out listening tasks” 4. Listening fatigue only occurs when the conscious allocation of mental resources has been overcome and the goal of the task has not been achieved. For these reasons, the FAS questionnaire is not designed to assess specific hearing abilities, but it may be affected by other coexisting conditions.
On the contrary, the EAS questionnaire is an assessment of a specific hearing ability. This concept is also emphasised and specified by the absence or weak correlation between EAS-IT and FAS-IT correlation in the 4 groups. The degree of listening effort or fatigue is also not related to anamnestic factors such as age at the time of administration of the questionnaires or gender. In line with our data, Alhanbali et al. found no significant difference in questionnaire scores between males and females and no correlation with age in any group 9. However, a correlation between the degree of hearing loss and age has been reported in the literature, with an increase in the degree of hearing loss with age 20.
A limitation of this study was the evaluation of CI patients with bilateral hearing loss but using only one device. It will be helpful to evaluate differences in listening effort between patients with one or 2 CIs implanted either simultaneously or sequentially. It will also be helpful to investigate and correlate the age of patients and the presence of disabilities with particular attention to cognitive impairment.
Conclusions
In conclusion, low internal consistency between items and low sensitivity between different types of hearing loss make the FAS-IT questionnaire an inconsistent tool for assessment of hearing-impaired listeners. On the other hand, the EAS-IT showed good internal reliability and validity and is sensitive to the effect of hearing loss. We conclude that the EAS and EAS-IT are reliable and consistent instruments in the Italian and British populations. This suggests the usefulness of the EAS-IT questionnaires for both clinical and research purposes.
Conflict of interest statement
The authors declare that they have no conflicts of interest.
Funding
This study is not sponsored and has not received external funding.
Author contributions
DC, SG: conceptualization, visualization; SG: methodology; VV, PF: validation; PF, SG: investigation, writing-original draft preparation; SG: resources; VV: writing-review and editing; DS, VV: supervision. All authors have read and agreed to the published version of the manuscript.
Ethical consideration
This study was approved by the Institutional Ethics Committee (Ethics Committee of the ‘Area Vasta’ Emilia-Nord) (approval number 423/2021/SPER/AUSLPC; date of approval 22/06/2021).
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: November 22, 2023
Accepted: July 2, 2024
Figures and tables
Figure 1. Mean score of the EAS-IT (in black) and FAS-IT (in grey) questionnaires into 4 groups: hearing aids (HA), cochlear implant (CI), single sided deafness (SSD) and normal hearing (NH).
Figure 2. Score correlation between EAS-IT and FAS-IT in the 4 groups.
| Group | N | Male | Age | PTA | PTA |
|---|---|---|---|---|---|
| n (%) | mean (range) | Better ear mean in dB (range) | Worse ear mean in dB (range) | ||
| NH | 101 | 39 (38.6%) | 43.4 (21-77) | 13.3 (0-35) | 13.5 (0-31.2) |
| HA | 19 | 7 (39.6%) | 55.9 (19-81) | 65.7 (32.5-96.2) | 78.2 (46.2-110) |
| CI | 50 | 24 (48%) | 53 (18-78) | 95.4 (48.7-130) | 113 (82.5-130) |
| SSD | 19 | 5 (26.3%) | 51 (18-72) | 17.2 (10-30) | 118.4 (67.5-130) |
| Total | 189 | 75 (39.7%) | 50.8 (18-81) | ||
| NH: normal hearing; HA: hearing aids; CI: cochlear implant; SSD: single-sided deafness. | |||||
| If item dropped | ||
|---|---|---|
| Item-rest correlation | Cronbach’s α | |
| EAS_Q1 | 0.905 | 0.939 |
| EAS_Q2 | 0.881 | 0.941 |
| EAS_Q3 | 0.757 | 0.955 |
| EAS_Q4 | 0.916 | 0.937 |
| EAS_Q5 | 0.878 | 0.942 |
| EAS_Q6 | 0.792 | 0.951 |
| If item dropped | ||
|---|---|---|
| Item-rest correlation | Cronbach’s α | |
| FAS_Q1 | 0.654 | 0.810 |
| FAS_Q2 | 0.620 | 0.812 |
| FAS_Q3 | 0.553 | 0.820 |
| FAS_Q4 | 0.156 | 0.862 |
| FAS_Q5 | 0.696 | 0.806 |
| FAS_Q6 | 0.686 | 0.807 |
| FAS_Q7 | 0.687 | 0.809 |
| FAS_Q8 | 0.649 | 0.811 |
| FAS_Q9 | 0.652 | 0.809 |
| FAS_Q10 | 0.151 | 0.861 |
| FAS_Q1 | FAS_Q2 | FAS_Q3 | FAS_Q4 | FAS_Q5 | FAS_Q6 | FAS_Q7 | FAS_Q8 | FAS_Q9 | FAS_Q10 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FAS_Q1 | — | |||||||||||||||||
| FAS_Q2 | 0.600 | *** | — | |||||||||||||||
| FAS_Q3 | 0.399 | *** | 0.449 | *** | — | |||||||||||||
| FAS_Q4 | 0.133 | -0.039 | -0.004 | — | ||||||||||||||
| FAS_Q5 | 0.560 | *** | 0.650 | *** | 0.448 | *** | 0.060 | — | ||||||||||
| FAS_Q6 | 0.515 | *** | 0.516 | *** | 0.524 | *** | 0.106 | 0.587 | *** | — | ||||||||
| FAS_Q7 | 0.540 | *** | 0.542 | *** | 0.402 | *** | 0.080 | 0.587 | *** | 0.563 | *** | — | ||||||
| FAS_Q8 | 0.463 | *** | 0.460 | *** | 0.543 | *** | 0.024 | 0.511 | *** | 0.580 | *** | 0.622 | *** | — | ||||
| FAS_Q9 | 0.536 | *** | 0.534 | *** | 0.424 | *** | -0.006 | 0.639 | *** | 0.500 | *** | 0.682 | *** | 0.667 | *** | — | ||
| FAS_Q10 | 0.082 | 0.004 | 0.124 | 0.550 | *** | 0.030 | 0.129 | 0.014 | -0.015 | -0.065 | — | |||||||
| * p < 0.05; ** p < 0.01; *** p < 0.001. | ||||||||||||||||||
| EAS-IT score | FAS-IT score | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | N | Median | Mean | SD | Range | Median | Mean | SD | Range |
| NH | 101 | 8 | 12.7 | 12.3 | 0-50.8 | 18 | 16.1 | 6.5 | 4-29 |
| HA | 19 | 46 | 39.2 | 16.2 | 6-59.7 | 17 | 17.6 | 7.6 | 8-38 |
| CI | 50 | 36.5 | 36.6 | 11 | 9.6-60 | 11.5 | 13.2 | 5.7 | 0-26 |
| SSD | 19 | 40.1 | 37.2 | 12.7 | 13-58 | 18 | 18.1 | 4.7 | 9-27 |
References
- Aggarwal R, Green K. Cochlear implants and positron emission tomography. J Laryngol Otol. 2012;126:1200-1203. doi:https://doi.org/10.1017/S0022215112002241
- Kelley K, Littenberg B. Structured review of dichotic tests of binaural integration: clinical performance in children. Am J Audiol. 2018;27:156-166. doi:https://doi.org/10.1044/2017_AJA-17-0032
- Füllgrabe C, Sęk A, Moore B. Senescent changes in sensitivity to binaural temporal fine structure. Trends Hear. 2018;22. doi:https://doi.org/10.1177/2331216518788224
- Pichora-Fuller M, Kramer S, Eckert M. Hearing impairment and cognitive energy: the Framework for Understanding Effortful Listening (FUEL). Ear Hear. 2016;37:5S-27S. doi:https://doi.org/10.1097/AUD.0000000000000312
- McGarrigle R, Munro K, Dawes P. Listening effort and fatigue: what exactly are we measuring? A British Society of Audiology Cognition in Hearing Special Interest Group ‘white paper’. Int J Audiol. 2014;53:433-440. doi:https://doi.org/10.3109/14992027.2014.890296
- Ghiselli S, Cuda D. Objective assessment of the “listening effort” in audiology. Otorhinolaryngology. 2021;71:172-180. doi:https://doi.org/10.23736/S2724-6302.21.02373-2
- Noble W, Gatehouse S. Interaural asymmetry of hearing loss speech, signal, spatial and qualities of hearing scale (SSQ) disabilities and handicap. Int J Audiol. 2004;43:100-114. doi:https://doi.org/10.1080/14992020400050015
- Hughes S, Rapport F, Watkins A. Study protocol for the validation of a new patient-reported outcome measure (PROM) of listening effort in cochlear implantation: the Listening Effort Questionnaire-Cochlear Implant (LEQ-CI). BMJ Open. 2019;9. doi:https://doi.org/10.1136/bmjopen-2018-028881
- Alhanbali S, Dawes P, Lloyd S. Self-reported listening-related effort and fatigue in hearing-impaired adults. Ear Hear. 2017;38:E39-E48. doi:https://doi.org/10.1097/AUD.000000000000361
- Michielsen H, De Vries J, Van Heck G. Psychometric qualities of a brief self-rated fatigue measure: the Fatigue Assessment Scale. J Psychosom Res. 2003;54:345-352. doi:https://doi.org/10.1016/s0022-3999(02)00392-6
- Canete O, Nielsen S, Fuentes-Lopez E. Self-reported listening effort in adults with and without hearing loss: the Danish version of the Effort Assessment Scale (D-EAS). Disabil Rehabil. 2022;6:1-8. doi:https://doi.org/10.1080/09638288.2021.2022781
- Alhanbali S, Al Jasser A, Aboudi O. Establishing the reliability and the validity of the Arabic translated versions of the Effort Assessment Scale and the Fatigue Assessment Scale. Int J Audiol. 2022;29:1-6. doi:https://doi.org/10.1080/14992027.2022.2085195
- Hall D, Zaragoza Domingo S, Hamdache L. A good practice guide for translating and adapting hearing-related questionnaires for different languages and cultures. Int J Audiol. 2018;57:161-175. doi:https://doi.org/10.1080/14992027.2017.1393565
- Anthoine E, Moret L, Regnault A. Sample size used to validate a scale: a review of publications on newly-developed patient reported outcomes measures. Health Qual Life Outcomes. 2014;12. doi:https://doi.org/10.1186/s12955-014-0176-2
- Rouquette A, Falissard B. Sample size requirements for the internal validation of psychiatric scales. Int J Methods Psychiatr Res. 2011;20:235-249. doi:https://doi.org/10.1002/mpr.352
- Champely S, Ekstrom C, Dalgaard P. Pwr: Basic Functions for Power Analysis.; 2017.
- Field A. Discovering Statistics Using SPSS. Sage publications; 2009.
- Mitton T, Yancey K, Isaacson B. Audiometric and patient-reported outcomes in single-sided deafness cochlear implant recipients using the CIQOL-35. Otolaryngol Head Neck Surg. 2023;168:1156-1163. doi:https://doi.org/10.1002/ohn.162
- Burg E, Thakkar T, Fields T. Systematic comparison of trial exclusion criteria for pupillometry data analysis in individuals with Single-Sided Deafness and normal hearing. Trends Hear. 2021;25. doi:https://doi.org/10.1177/23312165211013256
- Shetty H, Raju S, Singh S. The relationship between age, acceptable noise level, and listening effort in middle-aged and older-aged individuals. J Otol. 2023;18:220-229. doi:https://doi.org/10.1016/j.joto.2023.09.004
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 907 times
- PDF downloaded - 206 times



