Audiology
Vol. 45: Issue 4 - August 2025
Socio-economic impact of cochlear implantation in adults: an Italian study
Abstract
Objective. To analyse the cost-effectiveness of unilateral cochlear implant (CI) surgery in Italian adults with post-lingual deafness, focusing on direct costs, Health Utilities Index (HUI), QualityAdjusted Life Years (QALY), and Incremental Cost-Effectiveness Ratio (ICER).
Methods. The analysis, from the Italian healthcare system perspective, included preoperative, surgical, hospitalisation, and postoperative costs. QALYs were estimated using the Italian Nijmegen Cochlear Implant Questionnaire (I-NCIQ) and Ontario Health Utilities Index Mark 3 (HUI-3). HUI-3 score changes were analysed with regression models in Stat View (v5.0.1, SAS Institute Inc). ICER was calculated as the incremental cost per QALY (in Euros/QALY) over the average patient’s lifetime.
Results. CI significantly improved I-NCIQ (p < 0.001) and HUI-3 scores (p < 0.0001). Average life expectancy at surgery was 21.2 years; the degrade factor was 0.97, yielding a lifetime gain of 2.717 QALYs. Direct costs amount to €19,467.65. Cost-utility analysis showed €7,165.13 per QALY, below the €30,000/QALY ICER threshold.
Conclusions. CI surgery is cost-effective based on QALY analysis. Although cost-effectiveness decreases with age, quality of life and health benefits are comparable to younger patients.
Introduction
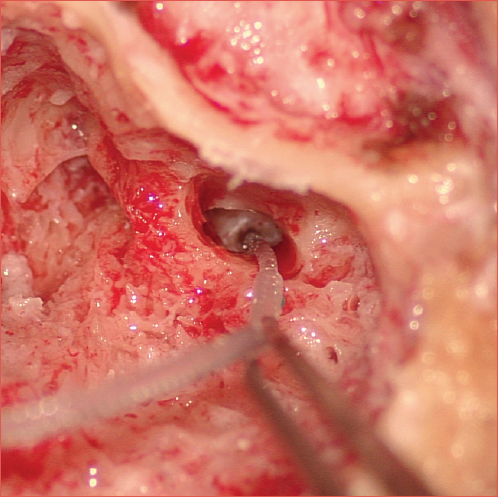
Hearing loss affects over one in 5 individuals and due to the increasing and aging population, the prevalence of hearing loss is expected to rise 1. In Italy, it is estimated that approximately 12% of the adult population, nearly 7 million individuals, is affected by hearing loss, of whom 21% experience severe to profound deafness. It is widely recognised that cochlear implants (CIs) can improve hearing in individuals with severe to profound sensorineural hearing loss who do not benefit from traditional hearing aids 2 (Cover figure). Evidence has extensively demonstrated the clinical effectiveness of CIs 2,3, as well as a positive impact on overall quality of life (QoL), reducing social isolation and discomfort, and enhancing speech, cognitive function, and community interaction 4. However, there persists a consistent undersupply of CIs relative to the proportion of potential recipients and, to date, a cost-effectiveness analysis has not been developed 5. In fact, only a few studies have conducted cost analyses in adults and the existing research demonstrates considerable heterogeneity, rendering cross-country comparisons unfeasible 6,7.
Cost-utility analyses quantify outcomes using Quality-Adjusted Life Years (QALYs), a key parameter for evaluating the effectiveness and efficiency of healthcare interventions 8. QALYs are computed by assigning a health state utility score to each life-year through widely used tools to measure QoL, such as the Health Utility Index (HUI) 9, providing a numerical assessment of an individual’s overall health, encompassing both physical and mental well-being. Thus, QALYs integrate both the quality and duration of life into a single metric 10.
The findings of a cost utility analysis are conveyed through the Incremental Cost-Effectiveness Ratio (ICER) 10 which juxtaposes the added costs of a new intervention with its added health benefits in comparison to the next best alternative. Costs are quantified in monetary units, while gains are measured in QALYs 11.
The most significant findings that emerged from a recent European review on the cost-analysis of CIs in adults indicate a favourable cost-effectiveness for unilateral CI, despite considerable heterogeneity observed in both healthcare systems and country-specific ICER thresholds 6. In fact, the commonly applied ICER threshold is $50,000, but recently a shift to higher numbers has been discussed and often recommended 12.
The World Health Organization (WHO), within its Commission on “Macroeconomics and Health”, states that the value of a gained year of life is approximately 3 times the per capita gross domestic product (GDP) 13. Given an Italian per capita GDP of approximately €30,000 14, each potentially life-saving intervention costing less than about €90,000 should represent a reasonable incremental cost for gaining an additional year of life in Italy. However, guidelines from the Italian Health Economics Association suggest reference values between €25,000 and €40,000 per QALY 15. Discrepancies in the value of a gained year of life, compared to that calculated using WHO methodology, highlight the variation in incremental cost-effectiveness thresholds among countries, which do not consistently correspond to per capita GDP 15.
A previous health technology assessment study 16 conducted in Italy suggested that unilateral CI are cost-effective in adults with a cost/QALY ranging from €24,000/QALY to €32,000/QALY compared to no intervention for patients with post-lingual deafness. However, due to a limited availability of economic studies, data were extrapolated from only 4 articles selected to assess the costs and benefits of CI in adults (2 conducted in the UK, one in France and one in the USA). The authors recommended to provide further insights into the cost-effectiveness of unilateral and bilateral CIs, highlighting the need to identify the substantial costs borne by local Italian healthcare systems.
Therefore, the objective of this research was to conduct a local cost-effectiveness analysis of unilateral CI surgery in post-lingually deafened adults, focusing on estimating direct costs, HUI, and QALY specifically in the context of Italy.
Materials and methods
To obtain an accurate estimate of direct costs, the target population was identified and comprised adults with severe to profound post-lingual hearing loss who were candidates for CI and underwent unilateral surgery at the Clinic of Otolaryngology, University of Trieste. According to patient candidacy criteria for CIs set by national guidelines, eligibility for a CI requires the patient to have severe or profound hearing loss, measured using the Pure Tone Average cut-off threshold of 0.5, 1, 2, and 4 kHz ≥ 75 dB HL in the better hearing ear, speech intelligibility ≤ 50% on speech audiometry using a traditional aid and to have no comorbidities that may affect the intervention 16,17.
A total of 57 adult patients (34 males and 23 females) were observed, with a mean age of 65 years and an age range from 24 to 90 years. The qualification criteria for CI align with the national guidelines and subsequent follow-up care.
Considering broad time horizons would require the use of fixed discount rates to make future values comparable at the same point in time. Costs and outcomes were discounted at 3% per year, following economic evaluation recommendations for Italy 18. Additionally, discount rates of 3% and 5% were included in the sensitivity analysis to facilitate cross-country result comparisons, following the recommendations of The Panel on Cost-effectiveness in Health and Medicine 19.
CIs are publicly funded in Italy and the cost parameters were collected for the year 2023 in a public tertiary referral hospital setting in Italy. The country population in 2022 was estimated to be 58.4 million. Life expectancy is 81.1 years for men and 85.2 years for women. All costs and benefits are expressed in euro per person and are aggregated over the expected lifetimes of patients following implantation, according to national life expectancy tables.
Direct costs
The direct cost parameters of CI surgery were collected in a public tertiary referral hospital setting in Italy and they were evaluated in collaboration with the Planning and Management Control Office of the University Health Authority. The base case analysis was conducted from the perspective of the Italian health care system. Direct surgery costs, audiology costs, and rehabilitation costs were included in the analysis and grouped as follows:
- preoperative assessment and patient’s preparation for surgery: specialist consultations, audiological hearing and speech assessments, imaging and biochemical blood tests;
- surgical and hospitalisation costs: direct and overhead costs for ward, nursing, other clinical staff, pharmacy, imaging, theatre, hospital bed costs, as well as implant and sound processor costs;
- postoperative services: fitting and programming of sound processor, specialist follow-up consultations for the first year.
On the basis of expert opinion 2 and in according to the literature 7, it was predicted that adults would participate in 6 pre-assessment appointments, which would involve consultations with both surgeons and audiologists for speech and hearing evaluations. Additionally, there were expected to be 10 post-surgical visits during the initial year, encompassing 2 follow-up care sessions with surgeons and 8 sessions with audiologists for targeted hearing and speech therapy 20. It was further assumed that all patients would attend one annual visit thereafter.
Health utility assessment and QALY evaluation
To assess the quality of life, the Italian Nijmegen Cochlear Implant Questionnaire (I-NCIQ) was extrapolated from each patient’s schedule, as it is routinely administered before and after surgery. This is a validated, self-administered tool that evaluates various aspects of a recipient’s functional abilities, psychological well-being, and social interactions. It consists of 60 items divided into 6 subdomains: Basic Sound Perception, Advanced Sound Perception, Speech Production, Self-esteem, Activity, and Social Interactions. Each item is rated on a 5-point Likert scale, providing a comprehensive overview of the impact of CI on the daily lives of patients.
Alongside it, the Ontario Health Utilities Index Mark 3 system (HUI-3), which is a generic, multi-attribute, preference-based questionnaire system, was used as a quantitative measure of general health status 8. Patients were initially prompted to recall their well-being status 4 weeks before CI surgery and were subsequently tasked with articulating their present health condition. The responses obtained from the HUI-3 survey were transformed into a HUI score, spanning from 0.00 (representing deceased) to 1.00 (indicating optimal health). Single-attribute utility scores were communicated using a spectrum from 0.00 (indicating a deficiency in function) to 1.00 (indicating complete functionality).
The calculations of cost-effectiveness were based on the QALY, national life expectancy tables and cost setting.
The relationship between changes in HUI-3 scores was analysed using regression model statistics in the Stat View for Windows (version 5.0.1, SAS Institute Inc). Pre- and post-implantation HUI-3 scores were statistically compared using the paired t-test.
To examine the correlation of QALYs with patient age, the sample was divided into age groups: 20-49, 50-69, and 70-90 years.
The ICER was then calculated resulting in a value that represents the incremental cost per QALY (in Euros/QALY). The ICER was calculated for each combination of age group. The time horizons are age and gender dependent and represent the individuals remaining life expectancy. All the costs and health utility values were calculated over the patient’s expected lifetime. Finally, Pearson’s correlation was used to assess the relationship between ICER and the variable ‘age’ in the entire sample, as well as in the subgroup of patients who had been using hearing aids (HAs) for more than 10 years. Additionally, the correlation within this latter subgroup was further analysed by splitting the sample based on age, using a cut-off of 70 years.
Results
The sample characteristics are reported in Table I. CI is linked to a notable improvement in QoL, as indicated by both the I-NCIQ and the HUI-3 assessments, for individuals aged 24 to 90 years (mean age ± SD, 63.4 ± 8.6 years). The I-NCIQ scores increased significantly from a preoperative average of 24.66 (SD ± 6.68) to a postoperative average of 61.27 (SD ± 10.469), with a statistically significant mean difference of 30.38 (SD ± 16.8) (p < 0.001). Figure 1 illustrates the gain in terms of I-NCIQ average scores. Similarly, the HUI-3 scores rose from a preoperative average of 0.37 (SD ± 0.26) to a postoperative average of 0.61 (SD ± 0.25), showing a statistically significant mean difference of 0.17 (paired t-test, t = -5.07 [p < 0.0001]).
A naïve regression did not yield any statistically significant results, indicating that the HUI3 gain was not associated with gender, age, side of the treated ear, nor was the HUI3 gain associated with the duration of hearing loss (p > 0.05).
Figure 2 reports the distribution of gains in HUI scores in relation to the age.
According to the ISTAT-life table, the average life expectancy of the sample estimated at the time of surgery was 21.2 years; the degrade factor was 0.97, thus in our cohort the average lifetime gain resulted in 2.717 QALY.
Cost-utility analysis
This increase in HUI-3 score was estimated to decline by 3% annually, leading to a projected cumulative gain of 2.717 quality-adjusted life-years (QALYs) over the remaining 21 years of life. The expenditures associated with CI amount to €19.467,65 encompassing pre-surgical assessments, the device’s cost, fees for surgeons and anaesthesiologists, hospital expenditures, and postoperative services, including programming and miscellaneous hardware costs (the details are reported in Table II). The cost-utility analysis yielded €19,467.65 for 2.717 QALYs, resulting in €7,165.13 per QALY. This value is below the commonly applied ICER threshold of approximately €30,000 per QALY.
Figure 3 illustrates the average QALY value per subgroups categorised by age.
In addition, Figure 4 depicts the ICER as a function of age at intervention.
The ICER curves were extrapolated, with the Y-axis representing the ICER (the cost of one QALY gained) in relation to age at intervention (X-axis).
The orange lines delineate the ‘zone of affordability,’ representing costs below €30,000.
Finally, the variable “age” was found to be significantly correlated with ICER in both the entire sample (p < 0.001) and the subgroup of patients who had been using HAs for more than 10 years (p < 0.05). In this latter subgroup, a cut-off of 70 years was used to differentiate elderly patients from those younger than 70. However, the correlation lost its statistical significance in both age-divided groups (p > 0.05). Similarly, in the subgroup of HAs non-users, no statistically significant variation in ICER was observed with increasing age (p > 0.05). The results are reported in Table III.
Discussion
The current cost-analysis for unilateral CI surgery in post-lingually deafened adults revealed a positive net benefit, incorporating both health utility and QALY gains. Specifically, no significant differences emerged in terms of HUI gain concerning the age of patients, according to Rohloff et al.21 However, the gain in QALYs exhibited an inverse relationship with age. This result is not surprising, considering that the calculation of QALYs is influenced by life expectancy. The correlation between age and ICER demonstrated a strong relationship in the overall sample, as well as in the subgroup of patients who had been using HAs for more than 10 years. However, this significance was lost when the subgroup was stratified with a 70-year cut-off.
This suggests that in the subgroup of patients who had been using HAs for more than 10 years, an increase in age did not correspond to a proportional rise in ICER. A similar observation was made in the subgroup of patients who were non-users of HAs. What is more surprising, however, is that even in cases of advanced age, the ICER remained below the willingness-to-pay threshold set at €30,000, except for an outlier case (Fig. 4). In this analysis, the cut-off was cautiously fixed at €30,000 although the trend in Europe is to set a higher spending threshold 10,19.
While the literature extensively analyses the impact of CI on a patient’s QoL, auditory gain, and sociability, little has been said about the country-related cost-effectiveness that should take into account GPD, health system context and reimbursements.3
Unilateral CI cost-effectiveness in adults has been assessed through some cost-benefit analyses, indicating improvements ranging from $7,000 to $40,000 per QALY, although the sources of information used for cost collection were not uniform nor universally declared. The results in our cohort align with findings from other countries, although direct comparisons are notably challenging.
In the UK, a recent study estimated cost-effectiveness through probabilistic sensitivity analysis and modelling. The study concluded that unilateral CI improved QoL and QALYs compared to traditional aids. However, it highlighted discrepancies among methodologies as a limitation 19.
Neve et al. 22 introduced the lifetime societal costs concluding that unilateral CI compared to hearing aid is more expensive, but with a 92% likelihood of being also cost-effective; it is important to underline that the value of the likelihood percentage varies at the varying of the cost-effectiveness threshold fixed in the analysis. The main obstacle in comparing monetary values across countries arises from this factor. An essential aspect to consider is that differences in eligibility criteria for CI contribute to discrepancies in outcomes. As a result, disparities in ICERs may not solely indicate economic differences but also variations in study methodologies.
Another significant aspect to consider in CI surgery is the age at which the patient is treated, which poses a sensitive consideration. Neve et al. included 2 adult groups: one comprising working-age adults and the other consisting of retired seniors 22. The researchers observed that cochlear implantation at any point during the working-age years demonstrated a positive net benefit from a societal perspective, with early treatment following eligibility for cochlear implants yielding higher societal benefits 3.
According to the results of this research, in the group of seniors aged 70 and above, where productivity becomes less relevant, the QALY gain was lower due to the shorter life span. Consequently, the cost-effectiveness of cochlear implantation in this population was found to be lower compared to other age groups 22. Previous studies have explored employment rates and income growth following CI, revealing that individuals under the age of 45 years are more prone to experiencing an increase in income post-CI. These findings imply that the timing of the implantation in a person’s lifespan plays a crucial role, indicating that earlier implantation is associated with a higher likelihood of individuals being able to secure or return to employment 29. The optimal duration of benefit from cochlear implants in elderly patients, especially in terms of cost-effectiveness, remains an area of concern. In a Swiss study, the authors investigated the impact of age in terms of cost-effectiveness of CI in adults and, even though the comparison was unilateral versus bilateral, they analysed health utility values taken from literature and representing values for an average study population. From a medical point of view, CI in the elderly is notoriously highly effective 21.
However, as the QALY is directly influenced by the duration of the achieved benefit, the calculated cost-effectiveness depends on the remaining life expectancy 24. The guidelines for CI are evolving, and this expansion is expected to result in a substantial increase in the number of CI procedures performed in the elderly population 25. CI in individuals aged 80 years and above shows a significant improvement in auditory function, with generally safe outcomes and positive mental health outcomes, including a reduction in depression one year post-implantation.
Since the study was conducted on a limited cohort of subjects, subdividing participants into different groups based on age and traditional hearing aid usage resulted in smaller sample sizes, making some comparisons less reliable. Nevertheless, the data on direct costs were rigorously collected, avoiding any extrapolation from the literature. The study has been conducted following the main criteria to ensure uniformity with other European cost analyses, thereby facilitating comparability of outcomes, in accordance with a recent European review 6.
Conclusions
CI surgery is deemed a cost-effective intervention when evaluated through QALYs analysis. While the cost-effectiveness diminishes somewhat in seniors, the gain in terms of QoL and overall health is comparable to that observed in younger subgroups. As is highlighted, the cochlear implant procedure yields positive benefits over an extended 20-year timeframe and lays the groundwork for a broader social perspective analysis.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
Med-El GmbH and Advanced Bionics (AB) equally made unrestricted donations to the Department of Medicine, Surgery, and Health of the University of Trieste (nr. 4954/2022).
Author contributions
GT, AG, MT: conceptualization; VPA: methodology; LC, GV: software; AG, LC, GT: validation; ES, FU: investigation; SZ, GV: data curation; MT, GV, AG: writing-original draft preparation; GT, AG: writing-review and editing; VPA, GT: supervision. All authors have read and agreed to the published version of the manuscript.
Ethical consideration
Ethical exemption: the study is a cost-effectiveness analysis.
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
History
Received: June 28, 2024
Accepted: October 30, 2024
Figures and tables
Figure 1. Gain in I-NCIQ scores after CI.
Figure 2. Distribution of gains in Health Utility Index (HUI) scores in relation to the age.
Figure 3. Average QALY gain per subgroups categorised by age.
Figure 4. ICER as a function of age at intervention.
| Characteristic | Mean values | |
|---|---|---|
| Age (mean ± S.D.) | 63.4 ± 8.6 years | |
| Gender | 34 M; 23 F | |
| Deafness duration | 28.5 years (range, 5-65 years) | |
| HAs usage > 10 years | 30 | |
| HAs usage < 10 years | 10 | |
| HAs non-users | 17 | |
| Pre- and postoperative HUI scores (mean ± S.D.) | 0.37 ± 0.26; 0.61 ± 0.25 | 0.17 (p < 0.0001) |
| Pre- and postoperative I-NCIQ scores (mean ± S.D.) | 24.66 ± 6.68; 61.27 ± 10.469 | 30.38 ± 16.8 (p < 0.001) |
| HAs: hearing aids; HUI: Health Utility Index; I-NCIQ= Italian Nijmagen Cochlear Implant Questionnaire; SD: standard deviation. | ||
| 1. Assessment costs | 696.87 |
| Preoperative specialist consultations - initial | 100.38 |
| Specialist consultation | 55.56 |
| Audiology hearing assessment | 22.41 |
| Audiology speech assessment | 22.41 |
| Preoperative tests | 534.20 |
| Audiometric test | 12.60 |
| Brain MRI with contrast agent | 356.80 |
| CT scan of the ear and mastoids without contrast | 19.10 |
| Blood chemistry tests | 105.60 |
| Electrocardiogram | 15.00 |
| Chest X-ray | 25.10 |
| Preoperative specialist consultation - subsequent | 58.92 |
| Preoperative ENT consultation | 29.46 |
| Preoperative anesthesiological consultation | 29.46 |
| Preoperative other costs | 3.37 |
| 2. Surgery - costs | 16,283.51 |
| Surgical instruments and consumables | 581.31 |
| Operating room and postoperative costs | 15,702.19 |
| Operating and post-operating room staff | 637.14 |
| Cochlear implant | 15,000.00 |
| General services | 65.05 |
| 3. Patient hospitalisation costs (average 4 days) | 1544.09 |
| 4. Postoperative services (first year) | 943.18 |
| Processor fitting | 100.60 |
| Audiometric test | 12.60 |
| Audiology speech assessment | 179.29 |
| Audiology hearing assessment | 179.29 |
| Specialist consultation | 444.45 |
| General outpatient clinic costs | 26.95 |
| Total costs | 19,467.65 |
| Sample characteristics | Pearson’s correlation coefficient between age and ICER | p value |
|---|---|---|
| The entire sample | 0.493 | 0.003* |
| HAs users for more than 10 years | 0.484 | 0.019* |
| HAs users for more than 10 years and <= 70 years old | 0.310 | 0.38 |
| HAs users for more than 10 years and > 70 years old | 0.299 | 0.322 |
| HAs non-users of any age | 0.54 | 0.068 |
| HA: hearing aids; *: statistically significant. | ||
References
- Wilson B, Tucci D, Merson M. Global hearing health care: new findings and perspectives. Lancet. 2017;390:2503-2515. doi:https://doi.org/10.1016/S0140-6736(17)31073-5
- Forli F, Turchetti G, Giuntini G. Cochlear implant in prelingually deafened oralist adults: speech perception outcomes, subjective benefits and quality of life improvement. Acta Otorhinolaryngol Ital. 2017;37:416-422. doi:https://doi.org/10.14639/0392-100X-1493
- Bergman P, Lyxell B, Harder H. The outcome of unilateral cochlear implantation in adults: speech recognition, health-related quality of life and level of anxiety and depression: a one- and three-year follow-up study. Int Arch Otorhinolaryngol. 2020;24:E338-E346. doi:https://doi.org/10.1055/s-0039-3399540
- Nijmeijer H, Keijsers N, Huinck W. The effect of cochlear implantation on autonomy, participation and work in postlingually deafened adults: a scoping review. Eur Arch Otorhinolaryngol. 2021;278:3135-3154. doi:https://doi.org/10.1007/s00405-020-06490-x
- Sorkin D. Cochlear implantation in the world’s largest medical device market: utilization and awareness of cochlear implants in the United States. Cochlear Implants Int. 2013;14:S4-S12. doi:https://doi.org/10.1179/1467010013z.00000000076
- Gatto A, Tofanelli M, Valentinuz G. Cochlear implant cost analysis in adults: a European narrative review. Eur Arch Otorhinolaryngol. 2024;281:4455-4471. doi:https://doi.org/10.1007/s00405-024-08591-3
- Foteff C, Kennedy S, Milton A. Cost-utility analysis of cochlear implantation in Australian adults. Otol Neurotol. 2016;37:454-461. doi:https://doi.org/10.1097/MAO.0000000000000999
- Arnoldner C, Lin V, Bresler R. Quality of life in cochlear implantees: comparing utility values obtained through the Medical Outcome Study Short-Form Survey-6D and the Health Utility Index Mark 3. Laryngoscope. 2014;124:2586-2590. doi:https://doi.org/10.1002/lary.24648
- Turchetti G, Bellelli S, Palla I. Systematic review of the scientific literature on the economic evaluation of cochlear implants in adult patients. Acta Otorhinolaryngol Ital. 2011;31:319-327.
- Gumbie M, Olin E, Parkinson B. The cost-effectiveness of Cochlear implants in Swedish adults. BMC Health Serv Res. 2021;21. doi:https://doi.org/10.1186/s12913-021-06271-0
- Laske R, Dreyfuss M, Stulman A. Age dependent cost-effectiveness of cochlear implantation in adults. Is there an age related cut-off?. Otol Neurotol. 2019;40:892-899. doi:https://doi.org/10.1097/MAO.0000000000002275
- Neumann P, Cohen J, Weinstein M. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796-797. doi:https://doi.org/10.1056/NEJMp1405158
- Macroeconomics and Health: Investing in Health for Economic Development. World Health Organization; 2001.
- theOECD.
- Il valore della spesa sanitaria in Italia dal 1990 al 2016.
- Berrettini S, Arslan E, Baggiani A. Analysis of the impact of professional involvement in evidence generation for the HTA Process, subproject “cochlear implants”: methodology, results and recommendations. Acta Otorhinolaryngol Ital. 2011;31:273-280.
- Hermann R, Lescanne E, Loundon N. French Society of ENT (SFORL) guidelines. Indications for cochlear implantation in adults. Eur Ann Otorhinolaryngol Head Neck Dis. 2019;136:193-197. doi:https://doi.org/10.1016/j.anorl.2019.04.006
- Guidelines for economic evaluations in Italy: recommendations from The Italian Group of Pharmacoeconomic Studies. Drug Inf J. 2001;35:189-201.
- Cutler H, Gumbie M, Olin E. The cost-effectiveness of unilateral cochlear implants in UK adults. Eur J Health Econ. 2022;23:763-779. doi:https://doi.org/10.1007/s10198-021-01393-y
- Gatto A, Tofanelli M, Costariol L. Otological planning software-OTOPLAN: a narrative literature review. Audiol Res. 2023;13:791-801. doi:https://doi.org/10.3390/audiolres13050070
- Rohloff K, Koopmann M, Wei D. Cochlear implantation in the elderly: does age matter?. Otol Neurotol. 2017;38:54-59. doi:https://doi.org/10.1097/MAO.0000000000001262
- Neve O, Boerman J, van den Hout W. Cost-benefit analysis of cochlear implants: a societal perspective. Ear Hear. 2021;42:1338-1350. doi:https://doi.org/10.1097/AUD.0000000000001021
- Clinkard D, Barbic S, Amoodi H. The economic and societal benefits of adult cochlear implant implantation: a pilot exploratory study. Cochlear Implants Int. 2015;16:181-185. doi:https://doi.org/10.1179/1754762814Y.0000000096
- Hammond-Kenny A, Borsetto D, Manjaly J. Cochlear implantation in elderly patients: survival duration, hearing outcomes, complication rates, and cost utility. Audiol Neurootol. 2022;27:156-165. doi:https://doi.org/10.1159/000517315
- Overview| Cochlear implants for children and adults with severe to profound deafness | Guidance | NICE. Published online 2019.
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 722 times
- PDF downloaded - 116 times




