Head and neck
Vol. 45: Issue 5 - October 2025
Stapler-assisted total laryngectomy and hybrid primary puncture: analysis of functional results
Abstract
Objective. To describe a new surgical technique called Hybrid Primary Puncture in Stapler-assisted Total Laryngectomy and to retrospectively compare two groups of patients undergoing total laryngectomy (TL) with or without the use of stapler.
Methods. Retrospective analysis performed on 110 patients undergoing TL and voice prosthesis (VP) primary placement, divided into “stapler group” and “no-stapler group”. The two groups were compared in terms of pharyngocutaneous fistula (PCF) incidence and events related to voice rehabilitation (hypertonicity, voice quality, complications related to VP).
Results. No statistically significant difference (p > 0.05) was found in “stapler” and “no-stapler” groups analysing the incidence of PCF, the percentages of patients who developed hypertonicity and experienced complications in the use and management of the VP. Regarding the vocal quality, a Quality of Voice index of “good” was found in similar percentages of patients in the two groups. Stratifying the sample, no significant differences emerged between “stapler” vs “no-stapler” in salvage TL in any of the parameters investigated.
Conclusions. The new technique allows to exploit, without any additional risk, the potential of stapler and primary VP placement.
Introduction
The surgical stapler is one of the fundamental instruments, used in many surgical specialties, to perform a quick and safe suture. In head and neck surgery linear staplers are the most commonly used. Allowing a double alternating layer of metal staples and a quick and safe closure of the tissues, in fact, they are used during total laryngectomy (TL) to remove the organ with a closed technique.
Unlike the open technique, this allows laryngeal excision without opening the pharynx 1 with a significant reduction in the duration of the operation 2. The incidence of complications after stapled closure is comparable, if not lower, than that related to manual closure 1-5. It is fair to point out, however, that in the closed technique failure to visualise the tumour during resection may lead to a potential risk of inadequate surgical margins. For this reason, the use of the stapler for pharyngeal closure should be indicated only for endolaryngeal 2,3 tumours with anterior growth, while involvement of the posterior paraglottic space, with potential pharyngeal spread, is undoubtedly an exclusion criterion.
The neopharynx resulting from the suture should be airtight to avoid leakage, wide and functional enough to allow the passage of food and the production of alaryngeal speech. Loss of elasticity could cause lack of vibration of the pharyngo-oesophageal segment. Excessive muscle tone, on the contrary, could cause spasms. Both conditions are undesirable for swallowing and rehabilitation of speech after TL 6,7.
Over the last 30 years, tracheo-oesophageal (TE) voice has become the “gold standard” of voice rehabilitation after TL 8,9 thanks to the ability to speak immediately after surgery, the more rapid acquisition of fluent speech and the high success rate (80-100%) 10. This high and long-lasting success rate is ensured when a multidisciplinary team is committed to identifying and resolving all voice prosthesis (VP) and TE voice problems 11-13. Additional advantages in terms of functional results and lower complication rates have been demonstrated in primary punctures, i.e., contextual to TL. However, during the use of the stapler the pharyngo-oesophageal lumen is never visualised since the mechanical suture simultaneously determines the removal of the larynx and the closure of the pharynx. Until now, therefore, it was necessary to use endoscopic techniques using rigid oesophagoscopy to create the tracheoesophageal fistula 14,15 and perform the TE puncture. In this way, the procedure took on the technical characteristics of secondary positioning despite being in fact primary.
The main limitation of this technique, defined as “hybrid”, lies in the need to perform a rigid endoscopy on a newly reconstructed pharyngo-oesophageal tract. If on the one hand we know that stapler suture determines a greater consistency of the neopharynx, it allows the execution of rigid oesophagoscopy without compromising its integrity as well as a direct visualisation of the progression of the esophagoscope in the pharynx with immediate detection of any lesions/damage of the neopharynx and its immediate repair 2, the need to further minimise any risks has led us to develop alternative strategies.
In this regard, a new technical variant to perform a TE puncture avoiding rigid esophagoscopy on a freshly made suture has been devised 16. The goal of this Hybrid Primary Puncture in Stapler-assisted Total Laryngectomy is to simultaneously exploit the advantages of stapler suture and primary puncture, without additional risk of pharyngocutaneous fistula.
The main purposes of this paper were to describe the above-mentioned technique and to retrospectively compare both the incidence of pharyngocutaneous fistula (PCF) and functional outcomes (hypertonicity, VP-related complications, voice quality) in patients undergoing TL divided into two groups based on use or not of the stapler during surgery.
Materials and methods
Setting and participants
The present study is a retrospective analysis carried out on patients suffering from laryngeal cancer who underwent TL and VP placement, from 2012 to 2022, at the ENT Clinic of the Fondazione Policlinico Universitario A. Gemelli-IRCCS in Rome. Data collection and systematisation was carried out by re-evaluating medical records from the hospital archive and during follow-up visits using the Speed RO software. The data used for this study were collected retrospectively from existing data sources, and all procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Medical Ethics Committee of the Catholic University of the Sacred Heart (ID 6945).
All patients were staged according to the TNM classification adopted by the American Joint Committee on Cancer (AJCC) and the Union International Contre le Cancer (UICC) 17 based on clinical (cTNM), radiological (rTNM) and histological (pTNM) data. All patients with a histological diagnosis of squamous cell carcinoma of the larynx were included in the study. All patients had undergone bilateral neck dissection and primary VP placement. The exclusion criteria were: involvement of the posterior paraglottic space on CT, pharyngeal involvement, cases with different histotypes, non-oncological pathology, distant metastases, primary tumour not completely resectable, secondary laryngeal neoplasms of other sites, reconstructive surgery with free microvascular or pedicled flap, incomplete medical record. In the selected period, 214 patients were initially identified. One hundred and four patients were subsequently excluded from the analysis due to lack of useful information for the purpose of this study. Therefore, the analysed sample included 110 laryngectomised patients with VP, whose characteristics are reported in Table I. Among these 110 patients, 40% (43 patients) underwent pharyngeal closure using a stapler, while the remaining 60% (67 patients) received a manual, non-mechanical closure. In all patients undergoing manual closure, a longitudinal myotomy along the posterior midline of the cricopharyngeal muscle was performed. No median longitudinal myotomy was performed in cases of Stapler closure.
Study design
For each patient, data were collected regarding gender, age, stage and extent of the tumour, neck dissection, primary treatment, intraoperative data (type of pharyngeal suture), diabetes and nutritional status. Patients eligible for the study were divided into two groups: the “stapler group” including subjects who underwent pharyngeal closure performed with a mechanical suturing machine, and the “no-stapler group” including patients in whom a traditional procedure with manual suturing was performed. The two groups were compared in terms of postoperative data (PCF) and events related to voice rehabilitation (hypertonicity, voice quality, complications related to VP). A second analysis was then conducted, taking into consideration only patients who had undergone salvage TL following failure of primary radiochemotherapy, on a total of 19 patients. These subjects were also classified in the two groups (stapler/no-stapler) and compared on the same parameters of the first analysis.
New surgical technique: Hybrid Primary Puncture in Stapler-assisted Total Laryngectomy
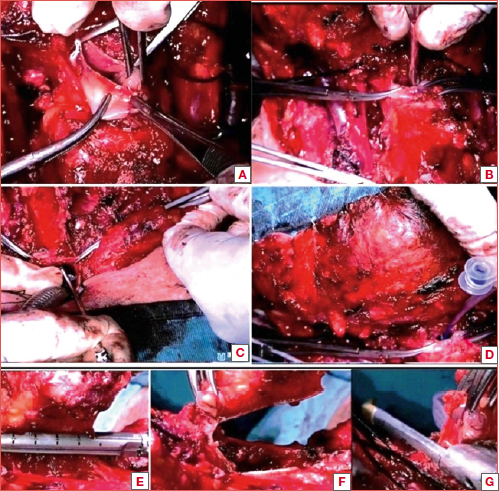
As already described in a recent paper of our group on the surgical technique 16, after extensive skeletonisation of the larynx, a horizontal cut of the selected cartilaginous tracheal ring is performed by sectioning up to the posterior tracheal wall, preserving the anterior wall of the cervical oesophagus intact. At this point, a 1 cm median horizontal pharyngotomy is performed. A Yankauer suction tube (without tip) is introduced into the oesophageal lumen toward the anterior oesophageal wall. The puncture is performed 5-10 mm from the upper edge of the posterior tracheal wall, previously incised during the laryngo-tracheal dissection. The flexible guidewire is introduced through the puncture needle into the lumen of the Yankauer suction tube which serves as a protector of the pharynx. The puncture needle is removed, a prosthesis of the appropriate size with the dilator is attached to the guidewire. The latter together with the dilator and the prosthesis is pulled out of the puncture opening. After insertion of the prosthesis, a vertical suture line is obtained using a 60-mm linear stapler (Covidien Endo GIA Articulating Reload with Tri-Staple Technology [60 mm]; Medtronic, Minneapolis, MN) oriented parallel to the oesophagus to allow proper closure. Therefore, to complete the suture of the pharynx, a horizontal suture line is performed using a 45-mm linear stapler (Covidien Endo GIA Auto Suture Universal Loading Unit [45 Å~ 3.5 mm]; Medtronic), reproducing the T-shaped repair (Fig. 1). This allows the suture at the base of the tongue to be strengthened, even when a macroscopic closure was obtained with the initial vertical suture. To create a watertight closure, an additional multilayer closure is performed: running interlocked suture with the pharyngeal fascia and residual pharyngeal constrictor muscle (second layer) and approximation of the strap muscles on the midline (third layer) to cover the neopharynx and to prevent hypotonicity. The entire surgical procedure is summarised in the Cover figure.
Outcomes
The two groups (“stapler” vs “no-stapler”) were compared in terms of PCF incidence, taking into consideration the onset of the fistula in both groups on the eighth and ninth posoperative day, assessed by methylene blue test. On the tenth postoperative day, in the absence of signs of PCF, the patients began oral feeding and phonatory rehabilitation.
The first functional outcome analysed was the hypertonicity of the pharyngeal constrictor muscle and residual cervical muscles. The severity of hypertonicity was also assessed by highlighting those patients refractory to basic rehabilitation techniques, in which it was necessary to perform an intramuscular infiltration of botulinum toxin to counteract the spasm.
Secondly, the incidence of VP-related complications was analysed. Specifically, the following complications were examined: persistent perivalvular leakage, repeated episodes of ingestion and/or extrusion of the VP, massive dilatations and/or granulations of the TE fistula. Intentionally, intravalvular leakage was not included as a complication because it was considered a natural evolution in the VP management.
To obtain a score that would allow to investigate voice quality, we created the Quality of Voice (QoV) Index. It originates from the combination of two tools that could summarise the patient’s self-assessment and the clinician’s perceptive judgment: the Italian version of Self Evaluation of Communication Experience after Laryngeal cancer (I-SECEL) questionnaire and the INFVo scale.
The I-SECEL 18 is a self-assessment questionnaire designed to measure self-reported adaptation to substitution voice and to the communication experiences and its purpose is to determine whether patients need specific counseling. A score of 36 ± 12 indicates a satisfactory level of adaptation. Scores above 60 indicate the need for psychological intervention.
The INFVo 19,20 is a scale specifically designed for clinician’s perceptual evaluation of substitution voices. The scale is made up of 4 parameters (I = overall impression; N = amount of unintended additive noise; F = fluency; Vo = quality of voicing) which can be evaluated on a scale from 0 to 10. The higher the score, the better the vocal outcome. The parameters we took into consideration when designing the new score were the I of the INFVo and the total score of the I-SECEL.
A combination of I > 5 and an I-SECEL score < 48 was considered “good”, a combination of I < 5 and an I-SECEL score > 48 was considered “bad”. All intermediate combinations (I < 5 and I-SECEL < 48; I > 5 and I-SECEL > 48) were considered “weak”.
Statistical analysis
Data was collected using Excel® 2016 (Microsoft, Redmond, WA, USA). Statistical analysis was performed using XLSTAT software version 2021.1. The statistical test used to analyse the data was the Chi Square with Yates correction. To verify the homogeneity of the two groups, the continuous numerical data, expressed as mean and standard deviation, were analysed using the Student’s t-test. The Mann-Whitney U test and Fisher’s exact test were used for categorical data. The significance level was set at p < 0.05.
Results
Regarding the incidence of PCF, this occurred in 16 patients of the entire sample (n = 110) (14.5%) and appeared between the 5th and 15th postoperative day (mean, 10.2±3.4 days). Twelve cases were primary laryngectomies (13.1%) and 4 were rescue laryngectomies (21%). The incidence of fistula in “stapler” and “no-stapler” groups was 13.9% (6/43 patients) and 14.9% (10/67 patients), respectively (p > 0.05). In the “stapler” group, fistula closure was obtained by local wound dressing in 4 patients, by internal mammary artery perforator (IMAP) flap in one patient, and by lipofilling in one patient. In the “no-stapler” group, fistula closure was obtained by local wound dressing in 7 patients, by IMAP flap in 2 patients and by lipofilling in one patient. Thirty-six out of 110 (32.7%) patients showed hypertonicity. Thirty-one cases were primary laryngectomies (34%) and 5 were rescue laryngectomies (26.3%). The incidence of hypertonicity in the “stapler” and “no-stapler” groups was 32.5% (14/43 patients) and 32.8% (22/67 patients), respectively (p > 0.05). Similarly, no statistically significant difference was found when analysing the percentages of patients who developed severe hypertonicity/spasm requiring botulinum toxin infiltration (5 out of 110, 4.5%: respectively 2/43, 4.6%, in the “stapler” group vs 3/67, 4.4% in the “no-stapler” group). Twenty out of 110 (18.1%) patients experienced VP-related complications (16/20, 17.5% in primary laryngectomies vs 4/20, 21% in salvage laryngectomies). The difference between “stapler” and “no-stapler” group was not statistically significant (p > 0.05) (6/43, 13.9% vs 14/67, 20.8%, respectively). Regarding vocal quality, the “stapler” group showed a “good” QoV index in 25/43 (58.1%) patients, a “weak” QoV index in 14/43 (32.5%) and a “bad” QoV index in 2/43 (4.6%) patients. The “no-stapler” group obtained a “good” QoV index in 40/67 (61.1%) patients, a “weak” QoV index in 24/67 (35.8%) and a “bad” QoV index in 3/43 (4.4%). The differences between the two groups were not statistically significant.
Rescue laryngectomies
By stratifying the sample and analysing only patients undergoing salvage laryngectomy (n = 19), no significant differences emerged between the “stapler” (n = 11/19, 57.8%) and “no-stapler” (n = 8/19, 42.1%) groups in any of the parameters investigated. All investigated parameters divided into “stapler” vs “no-stapler” and in primary vs rescue laryngectomy are summarised in Table II.
Discussion
Primary or salvage TL is performed in 30-35% of patients with locally advanced laryngeal cancer 21. Over the years, the use of the stapler for pharyngeal closure during TL, has fluctuated 22. This procedure must be reserved for cases in which the endolaryngeal and the anterior location of the tumour has been confirmed (the possibility of its use in tumours extending to the suprahyoid epiglottis, the piriform sinuses and the retrocricoid region is excluded) 23. Previous studies have shown that its use, in salvage laryngectomy also, is superior to manual suturing in reducing operating times and the length of hospital stay, thanks to an earlier start of oral feeding and the reduced incidence of PCF 2,24-25. Whether stapler suture is a cost-effective solution or not is out of the scope of the present study designed to analyse the reliability and safety of the technique associated to primary puncture, but these indirect costs could counterbalance the extra-costs of the stapler technique. Other studies in the future, focused on this specific topic, should confirm this hypothesis.
In a previous paper of our group 2, a primary VP placement was described together with the use of the stapler, but with a rigid oesophagoscopy immediately after the mechanical suture, as mentioned by other authors 23,26. Although this technique may expose the neosuture to the risk of injury, direct visualisation allows for immediate resolution, since compared to the pure secondary technique, the operating field is always open and it is possible to better control the procedure. The assumption of this intrinsic risk was dictated by the functional advantages that primary placement brings compared to the secondary one. Nevertheless, to further reduce the risk of damage to the new suture in all our patients undergoing stapler closure and candidate for VP rehabilitation, the new technique herein defined as Hybrid Primary Puncture in Stapler-assisted Total Laryngectomy has become the standard through a superior minipharyngotomy that allows to systematically perform retrograde VP positioning, without the use of rigid oesophagoscopy. In this retrospective analysis, the first parameter analysed was the incidence of PCF. The result obtained highlighted a non-significant difference between the two “stapler/no-stapler” groups, allowing any correlation with the type of suture performed to be excluded. By selectively studying patients undergoing salvage laryngectomy, also divided into the two “stapler/no-stapler” groups, we found similar results. Then, VP-related complications and voice outcomes were investigated. No significant difference was found when comparing the percentages of subjects, in the two distinct groups, who experienced hypertonicity and/or pharyngo-oesophageal spasm, both mild (resolvable with speech therapy) and more severe (requiring botulinum toxin infiltration). It is possible to assume that the use of the mechanical stapler does not cause hypertonicity of the constrictor muscles and residual cervical muscles. Hypertonicity represents an important risk factor because is often responsible for failure of the prosthetic rehabilitation 27. The new score created, called Quality of Voice (QoV) index and born from the combination of the I-SECEL total score and the I parameter (Global Index) of the INFVo scale, allowed us to investigate the voice outcomes. As observed in the other functional results, the closure technique used did not cause statistically significant differences. In fact, the percentage of patients who obtained a “Good QoV index” was comparable in the two groups analysed. Finally, with a view to easier patient management, the incidence of VP-related complications is an important parameter to evaluate. These complications, in fact, still constitute one of the main causes of reluctance shown by some clinicians in implementing this rehabilitation method 11. From the results obtained it is possible to state that there are no statistically significant differences between the two groups of patients examined and that, therefore, the use of mechanical stapler does not lead to an increase in late complications.
Considering salvage laryngectomy as an additional risk factor for the development of functional issues, the sample was stratified and analysed taking into consideration exclusively patients undergoing surgery after radiotherapy failure. Even in this subgroup of patients, mechanical suture did not determine significant differences compared to manual closure. It is therefore confirmed that the use of stapler, strictly adhering to the indications, seems to constitute an added technical value in the execution of TL, even in case of salvage surgery.
Conclusions
According to our results, stapler-assisted total laryngectomy, in selected cases, can be considered a safe and valid technique in both primary and salvage setting. The development of the new technique of hybrid primary puncture has made it possible to combine the use of the stapler with the simultaneous positioning of a VP, without additional risk for the pharyngo-oesophageal suture. This technique allows to benefit from the clinical advantages of mechanical closure, without giving up the already known functional advantages linked to primary placement and could represent a further incentive to use the stapler during TL.
Conflict of interest statement
All authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contributions
CP, JG: designed the work; CP, YL, GR, LP, MR, MCP, LD’A: acquired and analyzed data; CP, YL: drafted, and all authors revised the manuscript; JG: approved the last version.
Ethical consideration
All procedures performed in studies involving human participants were in accordance with the ethical standards of Ethics Committee “Università Cattolica del Sacro Cuore” (the study obtained the approval, ID 3181) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
History
Received: July 4, 2024
Accepted: March 23, 2025
Figures and tables
Figure 1. T-shaped repair.
| N = 110 patients | |
|---|---|
| Mean age (years) | 65.1± 6.5 years (range 33-83) |
| Sex | 93 M, 17 F |
| Closure | |
| Stapler | 43/110 (40%) |
| Manual | 43/110 (40%) |
| Surgery | |
| Primary | 91/110 (82%) |
| Salvage | 19/110 (18%) |
| Primary laryngectomy | Rescue laryngectomy | |||||
|---|---|---|---|---|---|---|
| (n = 91) | (n = 19) | |||||
| “Stapler” group | “No-stapler” group | “Stapler” group | “No-stapler” group | |||
| (n = 32) | (n = 59) | p | (n = 11) | (n=8) | p | |
| PCF incidence | 4 (12.5%) | 8 (13.5%) | NS | 2 (18.1%) | 2 (25%) | NS |
| Hypertonicity | 12 (37.5%) | 19 (32.2%) | NS | 2 (18.1%) | 3 (37.5%) | NS |
| Severe hypertonicity/spasm | 2 (6.2%) | 3 (5%) | NS | 0 (0%) | 0 (0%) | NS |
| VP complications | 4 (12%) | 12 (20.3%) | NS | 2 (18.1%) | 2 (25%) | NS |
| Good QoV Index | 19 (59.3%) | 35 (59.3%) | NS | 6 (54.5%) | 5 (62.5%) | NS |
| Weak QoV Index | 11 (34.3%) | 22 (37.2%) | NS | 5 (45.4%) | 2 (25%) | NS |
| Bad QoV Index | 2 (6.2%) | 2 (6.2%) | NS | 0 (0%) | 1 (12.5%) | NS |
References
- Öztürk K, Turhal G, Öztürk A. The comparative analysis of suture versus linear stapler pharyngeal closure in total laryngectomy: a prospective randomized study. Turk Arch Otorhinolaryngol. 2019;57:166-170. doi:https://doi.org/10.5152/tao.2019.4469
- Galli J, Salvati A, Di Cintio G. Stapler use in salvage total laryngectomy: a useful tool?. Laryngoscope. 2021;131:E473-E478. doi:https://doi.org/10.1002/lary.28737
- Dedivitis R, Aires F, Pfuetzenreiter E. Stapler suture of the pharynx after total laryngectomy. Acta Otorhinolaryngol Ital. 2014;34:94-98.
- Sannikorn P, Pornniwes N. Comparison of outcomes for staple and conventional closure of the pharynx following total laryngectomy. J Med Assoc Thai. 2013;96:S89-S93.
- Lee Y, Fang T, Kuo I. Stapler closure versus manual closure in total laryngectomy for laryngeal cancer: a systematic review and meta-analysis. Clin Otolaryngol. 2021;46:692-698. doi:https://doi.org/10.1111/coa.13702
- Zhang T, Cook I, Szczęśniak M. The relationship between biomechanics of pharyngoesophageal segment and tracheoesophageal phonation. Sci Rep. 2019;9. doi:https://doi.org/10.1038/s41598-019-46223-7
- Santoro G, Maniaci A, Luparello P. Dynamic study of oesophageal function during phonation: simple but effective. ORL J Otorhinolaryngol Relat Spec. 2021;83:304-309. doi:https://doi.org/10.1159/000513889
- Motta G, Galli V, Motta G. Surgical technics for implantation of tracheo-esophageal prosthesis in patients previously laryngectomized. Acta Otorhinolaryngol Ital. 1988;8:57-67.
- Motta G, Galli V, Tedesco S. Vocal rehabilitation of laryngectomized patients with tracheo-esophageal prosthesis. Original surgical technique in local anesthesia. Acta Otorhinolaryngol Ital. 1986;6:27-38.
- Cheng E, Ho M, Ganz C. Outcomes of primary and secondary tracheoesophageal puncture: a 16-year retrospective analysis. Ear Nose Throat J. 2006;85:264-267.
- Longobardi Y, Savoia V, Bussu F. Integrated rehabilitation after total laryngectomy: a pilot trial study. Support Care Cancer. 2019;27:3537-3544. doi:https://doi.org/10.1007/s00520-019-4647-1
- Salerno G, Villari P, Catalano V. Voice rehabilitation and quality of life in laryngectomized patients. Ann Ital Chir. 2023;94:7-10.
- Parrilla C, Longobardi Y, Paludetti G. A one-year time frame for voice prosthesis management. What should the physician expect? Is it an overrated job?. Acta Otorhinolaryngol Ital. 2020;40:270-276. doi:https://doi.org/10.14639/0392-100X-N0587
- Agrawal A, Schuller D. Closed laryngectomy using the automatic linear stapling device. Laryngoscope. 2000;110:1402-1405.
- Maves M, Lingeman R. Primary vocal rehabilitation using the Blom-Singer and Panje voice prostheses. Ann Otol Rhinol Laryngol. 1982;91:458-460.
- Galli J, Perna L, Rossi G. Hybrid primary puncture in stapler-assisted total laryngectomy. Head Neck. 2024;46:435-438. doi:https://doi.org/10.1002/hed.27571
- Brierley J, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumours. Wiley-Blackwell; 2016.
- Schindler A, Mozzanica F, Brignoli F. Reliability and validity of the Italian self-evaluation of communication experiences after laryngeal cancer questionnaire. Head Neck. 2013;35:1606-1615. doi:https://doi.org/10.1002/hed.23198
- Moerman M, Martens J, Crevier-Buchman L. The INFVo perceptual rating scale for substitution voicing: evelopment and reliability. Eur Arch Otorhinolaryngol. 2006;263:435-439.
- Schindler A, Ginocchio D, Atac M. Reliability of the Italian INFVo scale and correlations with objective measures and VHI scores. Acta Otorhinolaryngol Ital. 2013;33:121-127.
- Bozec A, Culié D, Poissonnet G. Current role of total laryngectomy in the era of organ preservation. Cancers (Basel). 2020;12. doi:https://doi.org/10.3390/cancers12030584
- Luk’ianchenko A. Suturing of a laryngeal defect in laryngectomy. Vestn Otorinolaringol. 1971;33:29-31.
- Altissimi G, Frenguelli A. Linear stapler closure of the pharynx during total laryngectomy: a 15-year experience (from closed technique to semi-closed technique). Acta Otorhinolaryngol Ital. 2007;27:118-122.
- Sanabria A, Olivera M, Chiesa-Estomba C. Pharyngeal reconstruction methods to reduce the risk of pharyngocutaneous fistula after primary total laryngectomy: a scoping review. Adv Ther. 2023;40:3681-3696. doi:https://doi.org/10.1007/s12325-023-02561-7
- Mandor E, Ebada H, El-Fattah A. Stapler versus conventional pharyngeal repair after total laryngectomy: a randomized clinical trial. Eur Arch Otorhinolaryngol. 2024;281:4273-4280. doi:https://doi.org/10.1007/s00405-024-08696-9
- Beswick D, Damrose E. Primary tracheoesophageal puncture and cricopharyngeal myotomy in stapler-assisted total laryngectomy. J Laryngol Otol. 2016;130:686-690. doi:https://doi.org/10.1017/S0022215116008070
- Parrilla C, Longobardi Y, Galli J. Periprosthetic leakage in tracheoesophageal prosthesis: proposal of a standardized therapeutic algorithm. Otolaryngol Head Neck Surg. 2021;165:446-454. doi:https://doi.org/10.1177/0194599820983343
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 522 times
- PDF downloaded - 181 times




