Head and neck
Vol. 45: Issue 5 - October 2025
Evaluation of the pan-immune-inflammation value in patients with Bell’s palsy
Abstract
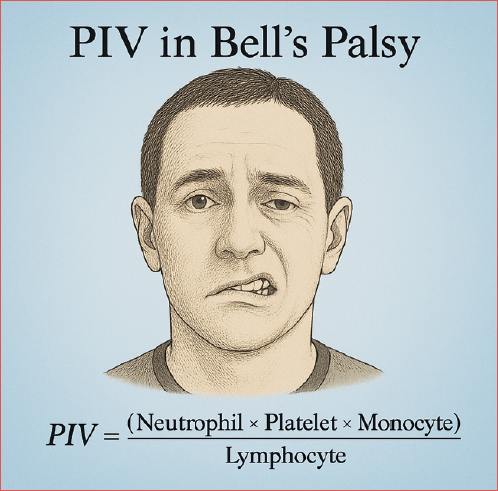
Objectives. Pan-immune-inflammation value is an inflammation index calculated using the parameters in a complete blood count (CBC) and has gained popularity in recent years. In this study, we aimed to examine its role in Bell’s palsy.
Methods. The study was designed as a retrospective case-control study. The study group consisted of 79 patients with Bell’s palsy. There were 158 patients in the control group. Age, gender, grade, CBC parameters and pan-immune-inflammation value were compared statistically between the groups.
Results. Leukocyte, neutrophil, platelet and pan-immune-inflammation values were significantly higher in the Bell's palsy group than in the control group (p values: < 0.001, < 0.001, 0.03, < 0.001, respectively). There was no correlation between grade of Bell’s palsy and any study parameters.
Conclusions. Our results support the theory that inflammation may be the main factor in pathogenesis, as the pan-immune-inflammation value is higher in patients with Bell’s palsy. Our results suggest that the cell group that plays a major role in this inflammation is neutrophils.
Introduction
Bell’s palsy is an idiopathic peripheral paralysis of the facial nerve. Diagnosis is made by excluding the possible aetiologies. It has been reported that 50% to 75% of peripheral facial palsy (PFP) are idiopathic. There is some evidence that herpes virus infections may play a role in the aetiology of Bell’s palsy. It is generally considered that inflammation is pivotal in its pathogenesis. The use of steroids and the response to this treatment also support the inflammation theory 1. Based on this situation, many studies have discussed the relationship between inflammation markers such as neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), systemic immune inflammation index (SII) and Bell’s palsy 2-5.
Pan-immune-inflammation value (PIV) is another indicator of systemic inflammation. PIV (neutrophil x platelet x monocyte/lymphocyte) is calculated using neutrophil, platelet, monocyte and lymphocyte counts. PIV is also known as aggregate index of systemic inflammation (AISI) 5. It is a relatively low-cost and easy-to-calculate index. It is evaluated both as a risk factor and as a prognostic factor in many pathologies such as colorectal cancer, breast cancer, malignant melanoma and vasculitis 6-9. In this study, we aimed to examine PIV in patients with Bell’s palsy.
Materials and methods
This retrospectively designed case-control type study was started by obtaining ethics committee permission number 149 dated 22.06.2023 from Süleyman Demirel University Faculty of Medicine Clinical Research Ethics Committee. The data were obtained from the files of patients diagnosed with Bell’s palsy between 01.01.2018 and 01.05.2023 at Süleyman Demirel University Faculty of Medicine, Department of Ear, Nose and Throat Diseases. Patients diagnosed with Bell’s palsy constituted the study group (each patient routinely underwent temporal bone contrast-enhanced magnetic resonance imaging and pure tone audiometry). A control group was created from patients who had septoplasty and/or rhinoplasty surgery on the same dates. Inclusion criteria for study group: no pathology other than PFP was detected in routine ENT and head and neck examination. The patient with Bell’s palsy must have a complete blood count and routine biochemistry examinations on the day he or she applies to our clinic and must be over 18 years of age. Exclusion criteria for study group: presence of central neurological findings accompanying PFP, history of head trauma before the development of PFP, known ear pathology, previous ear surgery, previous parotid surgery, history of malignancy, active infectious diseases, systemic inflammatory diseases, autoimmune disease history.
In parallel with the age and gender of the patients included in the study group, two patients were included in the control group for each patient in the study group, based on the order of admission and the following criteria. Inclusion criteria for the control group: no pathology was detected on the routine ENT and head and neck examination, no history of PFP, cranial base surgery performed before septoplasty and/or rhinoplasty operations. Exclusion criteria for the control group: history of previous PFP, history of malignancy, diagnosis of obstructive sleep apnoea syndrome, history of sinonasal infectious disease, presence of an active infectious disease, presence of a systemic inflammatory disease, presence of an autoimmune disease.
Statistical analysis
IBM SPSS 29 was used for statistical analysis of the data. Data were checked for data entry and distribution errors. Independent samples t test was used to compare continuous variables, and chi-square test was used to compare categorical variables. The correlation between grade parameter values and blood values was examined with Spearman’s rho correlation analysis. The results of categorical variables were presented as numbers and percentages, while the results of continuous variables were presented as mean and standard deviation. A value of p < 0.05 was considered statistically significant.
Results
There were 36 (45.6%) females and 43 (54.4%) males in the PFP group, and 72 (45.5%) females and 86 (54.4%) male in the control group. There were no significant differences between groups in terms of gender and age (p = 1.00 and p = 0.17 respectively). The mean age of the PFP group was 47.3 (± 17.5) years and the mean age of the control group was 44.8 (± 20) years. The paralysis was on the left in 43 patients and on the right in 36. Eleven (14%) of the patients had grade 2, 30 (38%) had grade 3, 25 (31.6%) had grade 4, seven (9%) had grade 5, and six (7.5%) had grade 6 PFP. Statistical comparison of the two groups in terms of blood parameters and PIV value is presented in Table I.
No correlation was detected between PFP grade and age, white blood count, neutrophil, lymphocyte, monocyte, platelet and PIV values (correlation coefficient: 0.041, -0.116, -0.095, -0.124, -0.133, -0.040, -0.043, respectively; p values: 0.71, 0.30, 0.40, 0.27, 0.24, 0.72, 0.70, respectively).
Discussion
Inflammation indices calculated from CBC have gained popularity in recent years. Since they are obtained by calculating more than one blood cell value, they are thought to be more meaningful than evaluating blood cells alone. In addition, their other advantages are that they are easy to calculate and have low costs. PIV is calculated using neutrophils, lymphocytes, platelets, and monocytes. For this reason, it is thought to represent inflammation more comprehensively than other indices 9. PIV is also called AISI in some studies 5. It has been addressed in various malignancies and inflammatory diseases 6-9. There is only one study in the literature examining the relationship between Bell’s palsy and PIV 5.
Bell’s palsy is the most common cause of PFP. It is characterised by idiopathic, acute, unilateral facial paralysis. Although viral infections, especially herpes viruses, are often blamed for its aetiopathogenesis, this has not been proven. It is believed that the main cause is oedema in the facial nerve. This oedema causes compression of the facial nerve in the fallopian canal 1. Regardless of the cause, it is thought that this oedema is associated with inflammation, and there are many studies in the literature examining patients with Bell’s palsy in terms of inflammation indices 2-5. In the study of Tuncer et al. they examined the relationship between Bell’s palsy and PIV, NLR, PLR, monocyte lymphocyte ratio (MLR); SII and systemic inflammation response index (SIRI) were also examined, in addition to CBC parameters. Among the listed indices, except MLR, they were found to be significantly higher in Bell’s palsy patients than in the control group. Among blood cells, neutrophils are significantly higher in patients with Bell’s palsy, while lymphocytes are lower than normal 5. The common point of the four significant indices is that lymphocyte is in the denominator. In addition, in PIV, NLR, SII and SIRI, neutrophils are in the numerator as well as lymphocytes in the denominator. In our study, PIV and neutrophil values were significantly higher in patients with Bell’s palsy, as in the study of Tuncer et al. Additionally, in our study, platelet levels were found to be higher in patients with Bell’s palsy. These results suggest that a mechanism related to the increase in neutrophils in peripheral blood may play a role in Bell’s palsy. In the study of Yılmaz et al., IL-6, IL-8 and TNF-α levels were found to be high in patients with Bell’s palsy 10. It is known that IL-6, IL8 and TNF-α play a role in activating neutrophils in the inflammatory response.11 In this respect, the results of Yılmaz et al. also support that neutrophilic inflammation may play a role in its aetiology 10.
In their study, Bucak et al. found neutrophil values and NLR in patients with Bell’s palsy to be significantly higher than in the control group. NLR was associated with poor prognosis in this study 2. In the study of Kınar et al., NLR and SII were found to be high in Bell’s palsy, and high SII was associated with poor prognosis 3. In the study of Eryılmaz et al., neutrophils and NLR were found to be high in paediatric Bell’s palsy patients. In that study, it was concluded that there is no correlation between the House-Brackman Classification and NLR 4. Our study is the first to examine the correlation between the grade of Bell’s palsy and PIV. For this reason, although a direct comparison cannot be made, in our study it was determined that there was no correlation between PIV and Bell’s palsy grade. Since NLR and PIV are expected to give parallel results, our result can be considered compatible with the study of Eryılmaz et al 4.
In the 2023 update of the Japanese Clinical Practice Guidelines for Bell’s Palsy, the use of systemic standard-dose corticosteroids is strongly recommended for the treatment of Bell’s palsy, regardless of disease severity. In this update, a standard dose is exemplified by 60 mg of prednisolone, while a high dose (weak recommendation) is exemplified by 120 mg of prednisolone. Other treatments are weakly recommended due to insufficient evidence. The guideline suggests that treatment approaches be decided based on the severity of the disease. Adding antiviral therapy to systemic steroids is weakly recommended, regardless of disease severity. Intratympanic steroid therapy in addition to systemic steroids is not recommended for mild-to-moderate cases, while it is weakly recommended for severe cases 12. The stronger recommendation for systemic steroids over intratympanic steroids and antiviral therapies in the updated guideline supports the role of systemic inflammation in the pathogenesis. In our study, PIV, an indicator of systemic inflammation, was found to be significantly higher in patients with Bell’s palsy. The relationship between PIV and treatment response could be explored in more comprehensive studies.
The main limitations of our study are the limited number of patients and the lack of prognosis evaluation.
Conclusions
The aetiopathogenesis of Bell’s palsy has not been determined. In recent years, studies examining Bell’s palsy patients in terms of inflammation indices have gained popularity. In our study, we found that PIV, neutrophil and platelet values were higher in patients with Bell’s palsy. These results can be interpreted as neutrophilic inflammation may play a role in Bell’s palsy. Our results need to be confirmed by further studies.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
MES, VA, HY, EO: concept, design, writing, data collection and processing, analysis and interpretation, literature search.
Ethical consideration
This study was approved by the Institutional Ethics Committee (Süleyman Demirel University Faculty of Medicine Clinical Research Ethics Committee) (approval number/protocol number 149/22.06.2023).
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki.
History
Received: February 11, 2024
Accepted: September 9, 2025
Figures and tables
| Control group | PFP group | p | |
|---|---|---|---|
| (n = 158) | (n = 79) | ||
| Mean ± SD | |||
| WBC | 7.09 (± 1.95) | 10.71 (± 4.14) | < 0.001 |
| Neutrophils | 4.17 (± 1.54) | 7.77 (± 3.84) | < 0.001 |
| Lymphocytes | 2.12 (± 0.57) | 2.20 (± 1.31) | 0.29 |
| Monocytes | 0.55 (± 0.18) | 0.58 (± 0.30) | 0.19 |
| Platelets | 247.85 (± 60.21) | 267.56 (± 76.98) | 0.03 |
| PIV | 311.85 (± 287.05) | 728.42 (± 1076.94) | < 0.001 |
References
- Baugh R, Basura G, Ishii L. Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg. 2013;149:1-27. doi:https://doi.org/10.1177/0194599813505967
- Bucak A, Ulu S, Oruc S. Neutrophil-to-lymphocyte ratio as a novel-potential marker for predicting prognosis of Bell palsy. Laryngoscope. 2014;124:1678-1681. doi:https://doi.org/10.1002/lary.24551
- Kınar A, Ulu Ş, Bucak A. Can Systemic Immune-Inflammation index (SII) be a prognostic factor of Bell’s palsy patients?. Neurol Sci. 2021;42:3197-3201. doi:https://doi.org/10.1007/s10072-020-04921-5
- Eryilmaz A, Basal Y, Tosun A. The neutrophil to lymphocyte ratios of our pediatric patients with Bell’s palsy. Int J Pediatr Otorhinolaryngol. 2015;79:2374-2377. doi:https://doi.org/10.1016/j.ijporl.2015.10.047
- Tuncer E, Kahraman M, Yuksel F. Which is the best inflammatory index in Bell’s palsy?. Tr-ENT. 2023;33:76-80. doi:https://doi.org/10.26650/Tr-ENT.2023.1285124
- Corti F, Lonardi S, Intini R. The Pan-Immune-Inflammation Value in microsatellite instability-high metastatic colorectal cancer patients treated with immune checkpoint inhibitors. Eur J Cancer. 2021;150:155-167. doi:https://doi.org/10.1016/j.ejca.2021.03.043
- Demir H, Demirci A, Eren S. A new prognostic index in young breast cancer patients. J Coll Physicians Surg Pak. 2022;32:86-91. doi:https://doi.org/10.29271/jcpsp.2022.01.86
- Susok L, Said S, Reinert D. The pan-immune-inflammation value and systemic immune-inflammation index in advanced melanoma patients under immunotherapy. J Cancer Res Clin Oncol. 2022;148:3103-3108. doi:https://doi.org/10.1007/s00432-021-03878-y
- Lee L, Ahn S, Pyo J. Pan-immune-inflammation value at diagnosis independently predicts all-cause mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Clin Exp Rheumatol. 2021;39:88-93. doi:https://doi.org/10.55563/clinexprheumatol/m46d0v
- Yilmaz M, Tarakcioglu M, Bayazit N. Serum cytokine levels in Bell’s palsy. J Neurol Sci. 2002;197:69-72. doi:https://doi.org/10.1016/s0022-510x(02)00049-7
- Wright H, Moots R, Bucknall R. Neutrophil function in inflammation and inflammatory diseases. Rheumatology (Oxford). 2010;49:1618-1631. doi:https://doi.org/10.1093/rheumatology/keq045
- Fujiwara T, Hato N, Kasahara T. Summary of Japanese clinical practice guidelines for Bell’s palsy (idiopathic facial palsy) - 2023 update edited by the Japan Society of Facial Nerve Research. Auris Nasus Larynx. 2024;51:840-845. doi:https://doi.org/10.1016/j.anl.2024.07.003
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 562 times
- PDF downloaded - 160 times




