Reviews
Vol. 44: Issue 5 - October 2024
The prognostic role of salivary miRNAs in oral squamous cell carcinoma: technical challenges and clinical perspectives
Abstract
In management of oral squamous cell carcinoma (OSCC), only a few biomarkers, ranging from clinical and histopathological features to molecular alterations, have been demonstrated to have clinical and prognostic utility. The intent of this narrative review is to present current findings on the use of salivary microRNAs (miRNAs) as prognostic oncologic biomarkers in patients with OSCC. The ability to predict survival or recurrence during follow-up by quantification of specific miRNAs in saliva has been shown in a number of studies, and serves as a possible feature to address in future well-designed clinical studies to confirm their prognostic value. The non-invasiveness of liquid biopsy techniques, the ease of saliva collection, and the abundance and stability of miRNAs in such a biologic fluid make it an attractive combination to improve management of OSCC. For salivary miRNAs to be used in routine practice, however, methodological and sampling standardisation are still needed to increase the power and accuracy of the results obtained.
Introduction
Oral squamous cell carcinoma (OSCC) is the most common tumour of the head and neck region. With a 5-year survival rate of around 50%, OSCC represents a significant cause of cancer-related death globally, especially in underdeveloped nations 1. This percentage varies greatly according to the clinical stage of disease at diagnosis and availability of the best diagnostic, therapeutic, and rehabilitative options. Surgery alone represents the standard of care for these tumours in their initial phases of development. However, in more advanced stages, OSCCs require aggressive multidisciplinary therapeutic approaches including surgical resection and reconstruction, followed by (chemo)radiotherapy, and frequently show an inexorably fatal course 2.
The molecular mechanisms underlying the intrinsic aggressiveness of OSCC remain largely unknown. Integrated pan-genomic studies conducted in OSCC have shown the convergence of specific alterations into distinct molecular subgroups 3. Although very informative from a biological perspective, the molecular subtypes of OSCC have not been associated with clinically relevant differences in outcomes, revealing the complexity and high intra-tumoural heterogeneity of OSCC. Consequently, despite the efforts made in the search for reliable prognostic molecular markers 4, response to treatment and post-therapeutic monitoring, at present risk stratification and survival prediction of OSCC still rely on traditional clinical and histopathological parameters such as TNM staging, in addition to histological assessment of grading, worst pattern of invasion, perineural, and lympho-vascular involvement 5.
With the advent of liquid biopsy (LB) as a minimally invasive method to gain insight into the biology and dynamics of the tumour from a patient’s fluid sample, new molecular markers have emerged. Originally referring exclusively to circulating tumour cells (CTC) in the blood of patients with cancer, the LB concept was later extended to other physiological fluids such as urine, bone marrow, saliva and cerebrospinal fluid, and now comprises different molecular entities like circulating cell-free DNA (cfDNA), circulating tumour DNA (ctDNA), RNA, including small non-coding RNA, and extracellular vesicles 6. Reflecting somatic alterations present in tumour tissue, LB-based biomarkers hold the potential for early detect cancer, monitor treatment response or disease progression. This value has been widely demonstrated in several cancer types, including OSCC, where increased levels of plasma cfDNA have been described in patients compared to controls, and correlated with clinicopathological features 7. More recently, the new idea of anticipating recurrence through cfDNA-based minimal residual disease (MRD) detection following curative treatment, already successfully pursued in other solid tumors 8, has also been applied to head and neck SCC (HNSCC), illustrating the feasibility of personalised LB-based assay for planning therapy and follow-up 9. Further supporting the prognostic capacity of LB, a serum-based miRNA classifier capable of identifying recurrent OSCC before it becomes clinically evident has been reported as a promising approach for non-invasive monitoring of OSCC 10.
With respect to conventional and/or targeted therapy the predictive value of circulating miRNA is emerging both in adjuvant and neoadjuvant settings. In HER-2 positive breast cancer patients, for instance, changes in plasma levels of specific miRNA have been associated with response to neoadjuvant trastuzumab-based therapy and exploited to differentiate among patients with distinct prognosis 11. Moving to the immune-checkpoint-inhibitor (ICI) context, ongoing investigations in advanced lung cancer are exploring how the profile of plasma or serum-derived miRNA correlates to checkpoint blockade response, with multiple baseline signature identified that could distinguish responders from non-responders 12. Such important findings encourage the study of miRNA-based LB to predict benefit from ICI therapy in OSCC as well, since immunotherapy has already shown promising efficacy in recurrent and metastatic diseases and is currently under investigation in the neoadjuvant/induction settings 13.
Recent studies indicate that saliva is more enriched with ctDNA compared to blood plasma in HNSCC 14 and suggest that the quantification of these molecules in saliva may aid in both diagnosis and treatment of patients with OSCC.
Saliva as a matrix for biomarkers
Because of its direct proximity to the oral cavity, saliva represents an easily accessible source of biomarkers, offering an inexpensive, non-invasive means to assess the presence and characteristics of OSCC. As for peripheral blood, saliva can provide information about the dissemination of disease in terms of circulating molecules mirroring the biological features of tumour cells from which they derived, and represent an alternative to current standard-of-care tissue biopsy 14. Hence, the analysis of saliva has the potential to provide useful information for early diagnosis of primary OSCC and recurrent disease, along with its prognostication 16. This possibility has been extensively explored in the last decades. The continuously growing number of published reports collectively suggests its feasibility for several clinical applications such as early detection, choice of treatment, and surveillance of OSCC, including the value of longitudinal LB for early detection of recurrence.
In the following paragraphs, the main studies with a focus on the use of salivary miRNA-based LB in OSCC prognostication will be presented.
Detection of miRNAs in saliva
Subtypes of RNA circulating in saliva include miRNAs, a class of single-strand, small, non-coding RNAs which play crucial roles in regulating varying cellular process, and exhibit differences in expression profiles between healthy individuals and those with disease which reflect differential expression patterns in cancer cells compared to normal ones 17. miRNAs are present in both whole saliva and supernatant, where they circulate as cf-miRNAs associated with RNA binding proteins or selectively packed in extracellular vesicles (i.e. exosomes) which protect them from degradation by endogenous ribonucleases.
Sufficient amounts of high-quality extracellular miRNAs can be isolated from saliva using commercial kits 18. A variety of profiling methods and analytical platforms, either based on real-time quantitative polymerase chain reaction (RT-qPCR), microarray or next-generation sequencing, are used to detect their levels of expression 19. Along with relative abundance and the remarkable stability of miRNAs in saliva, these properties fulfill the main requirements of an ideal biomarker defined as a measurable, objective indicator of an individual’s normal or pathological state, and strengthen the utility of salivary miRNAs as non-invasive biomarkers for diagnosis and monitoring of cancer. Distinct miRNA expression profiles have indeed appeared between saliva of OSCC patients and healthy controls in multiple independent studies. In addition, different levels of miRNA expression have been described in OSCC as a potential predictor of survival.
In one of the first studies comparing the expression levels of selected miRNAs in saliva between OSCC and healthy subjects, Park and colleagues 20 observed a significant decrease in miR-125a and miR-200a in patients with OSCC compared to control subjects. A diagnostic panel of 3 miRNAs was later developed by Salazar et al. 21 for the detection of HNSCC after validation in saliva samples from two independent cohorts of healthy controls and patients. This combination of miRNA provided a satisfactory diagnostic capacity (area under the curve [AUC] = 0.74, p < 0.0001) and indicated that salivary derived miR-9, miR-134, and miR-191 are novel biomarkers that can reliably detect HNSCC.
Rawi et al. 22 systematically reviewed the role of differentially expressed miRNAs in saliva as potential biomarkers in OSCC and, among 14 published studies, found 25 miRNAs that were differentially expressed between cases and controls. Of interest, 4 of these, namely miR-21, miR-31, miR-125, and miR-200, were evaluated in more than one study, supporting their relevance in this cancer type.
The results of a meta-analysis by Kang in 2021 23, which gathered data from 443 HNSCC patients and 316 healthy controls in 17 studies, reported an overall moderate level of accuracy of salivary miRNAs in discriminating between patients with cancer and healthy controls with a combined sensitivity and specificity of 0.697 (95% confidence interval [CI] = 0.644-0.744) and 0.868 (95% CI = 0.811-0.910), respectively, and an AUC of 0.803. Nevertheless, the results of individual studies indicate that several miRNAs used alone show excellent accuracy and clinical value. Expecting to define the most efficient method to combine miRNAs, together with the definition of an optimal cut-off value for expression and a common normalisation strategy, the authors highlighted the need for large-scale multicentre studies to validate these results.
The predictive and prognostic values of salivary miRNAs in OSCC
Unlike the diagnostic capacity of salivary miRNAs, their potential in predicting OSCC progression and/or anticipating post-treatment recurrence is emerging. In reviewing the current literature to verify the association of salivary miRNAs with survival in HNSCC, 4 publications were retrieved showing that miRNA expression has prognostic value.
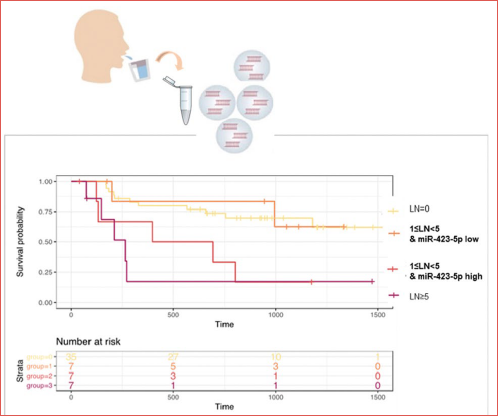
In a pioneering study conducted by our research group in 2021 24, we showed that increased expression of miR-423-5p in preoperative saliva from patients with OSCC independently predicted reduced disease-free survival (DFS), and when included in multivariate analysis with the number of positive lymph nodes (LN), it was the only feature strongly associated with DFS when considering purely clinical variables. The robustness of miR-423-5p was tested in two independent cohorts of individuals, in which miR-423-5p overexpression was also confirmed to be useful in subclassifying those patients considered in an intermediate-risk class according to the LN status (i.e. 1 ≤ LN < 5), and demonstrated that quantification of salivary miRNAs could also assist in prognostic stratification. In particular, patients with 1 to 5 positive nodes could be segregated according to the presence or absence of miR-423-5p in two groups, which showed survival outcomes similar to the high-risk (more than 5 positive nodes) and low-risk group (no positive nodes), respectively (Cover figure).
Enhanced expression of miR-1307-5p was also found exclusively in tissue and salivary exosomes isolated from patients with OSCC compared to non-cancerous counterparts, and demonstrated clinical association with chemo-resistance. In fact, a significant increase in the expression levels of salivary exosomal miR-1307-5p was observed in the chemo-resistant cohort (fold-change [FC] = 4.82 ± 2.38, p = 0.01) compared to patients with complete remission (FC = 2.3 ± 1.2) 25 making it an ideal prognosticator for OSCC.
Two papers, both published in 2023 26,27, more specifically evaluated the association of salivary miRNAs with clinical-pathological features or risk factors for HNSCC. Tailoring the study on the Indian population, Saproo and colleagues 26 identified miR-6087 and miR-449b-5p as potential salivary indicators of OSCC and functionally associated with multiple oncogenic pathways, including those related to drug response. In a pilot study performed on 23 patients with OSCC and 21 healthy volunteers, assessing salivary and serum miRNAs associated with OSCC and stratified by smoking status, salivary miR-21, miR-136, and miR-3928 all showed significant differential expression in early stage tumours versus controls (p < 0.05) 27. MiR-21, in particular, was detected at significantly higher levels in saliva of patients with OSCC and smoking history compared to patients with OSCC who had never smoked or healthy control smokers (p < 0.005). Thus, miR-21 in the saliva of current/former smokers is potentially associated with OSCC and is useful for risk stratification.
Translating salivary miRNAs in routine practice: obstacles and challenges
The non-invasiveness of LB techniques, the ease of saliva collection, and the abundance and stability of miRNAs in saliva make it an attractive combination to improve management of OSCC. In this field, the informative potential of extracellular miRNAs circulating in saliva has been explored for early detection, using quantitative assessment of key miRNAs and measuring changes in their expression levels. This is a novel notion that has been recently used in clinical research on other cancer types, including breast and lung cancer, and has also been proposed for risk stratification, monitoring the course of disease and the patient’s response to conventional and targeted treatments 28,29. Despite the undoubted advantages of miRNA-based salivary LB, its routine use in clinical practice has yet to be introduced and the fundamental reason is the high heterogeneity of existing research on this topic, which have not currently produced any validated miRNA, not even in the types of cancer where the research is more advanced.
From a methodological point of view, testing miRNAs in biofluid samples is challenging in many ways. Like other biofluids, saliva is susceptible to several pre-analytical variables, ranging from how samples are collected, processed, and stored to methods of extraction and quality control of the purified miRNAs 30. All these steps are considered to be potential causes of inconsistency in miRNA experiments that make comparison between studies and reproducibility of published data virtually impossible. At a prognostic level, in particular, considering the relatively small sample size of published studies and the lack of information on follow-up, the available data on salivary miRNAs in OSCC are still insufficient to draw significant conclusions about their possible utility in survival prediction. Biological factors further contributing to discrepancies between studies may be attributed to the composition of tumour microenvironment (TME), as alteration of miRNAs has also been demonstrated in stromal and immune cell population and could directly influence the expression of target miRNAs 31. This observation highlights the urgency of validating the most promising candidate miRNAs in large independent sample sets to minimise the effect of such potential confounding factor. Bioinformatic approaches could also be adopted to find specific miRNA profiles related to TME components, complemented by in vitro functional studies to identify tumour-specific signatures. Furthermore, in situ detection of miRNAs using recent RNAscope technology 32 could be useful to study their spatial expression profile in tissues.
Considering that RT-qPCR is the most commonly used method to detect miRNAs, the main challenge at the post-analytical level is definition of a proper normalization strategy, which is critical to overcome the intrinsic limits of this approach based on relative quantification of the levels of target miRNA compared to an endogenous reference 33. In fact, the choice of reference miRNA for qPCR data correction has a great impact on the results, since different normalisation strategies can lead to differences in interpretation of data, thus resulting in ambiguous or even contradictory conclusions. The emergence of complementary detection systems, such as droplet digital technology (ddPCR), may be a reliable alternative to RT-qPCR for the absolute quantification of circulating miRNAs 34. Applied to serum, ddPCR provided greater reproducibility and higher sensitivity in low-abundance miRNA detection compared to qPCR 35,36. In addition, being able to quantify the exact count of circulating miRNA without the need of normalization steps, and being more resilient to differences in sample quality, the ddPCR approach should simplify the comparison of results obtained in different studies and warrants further investigation in saliva.
Conclusions
The search for biomarkers that are useful in predicting prognosis or defining risk of recurrence is one of the fields that can potentially improve outcomes of patients with OSCC, and follow-up after treatment with curative intent has the main objective of detecting local recurrence as early as possible. After reviewing major studies that have evaluated the expression of circulating miRNAs as biomarkers in OSCC, there appears to be adequate evidence that LB techniques can be of tremendous benefit in clinical management. Circulating miRNAs can be obtained as a very stable biomarker in saliva, and may thus represent a more appropriate surrogate LB biomarker compared to other circulating components 37. Although few studies have explored the prognostic potential of miRNAs in saliva, the available results are encouraging. With the emergence of increasingly sensitive, reliable, and low-cost technologies to isolate and quantify circulating miRNAs, the analysis of such biomarkers is likely to become the next frontier in clinical management of OSCC.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
CR, CP: study conception and manuscript writing; DM, CA, VR: manuscript editing.
Ethical consideration
The study does not involve human or animal subject.
History
Received: February 23, 2024
Accepted: April 6, 2024
Published online: September 15, 2024
References
- Cunha A, Compton K, Xu R. The global, regional, and national burden of adult lip, oral, and pharyngeal cancer in 204 countries and territories: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2023;9:1401-1416. doi:https://doi.org/10.1001/jamaoncol.2023.2960
- Worthington H, Bulsara V, Glenny A. Interventions for the treatment of oral cavity and oropharyngeal cancers: surgical treatment. Cochrane Database Syst Rev. 2023;8. doi:https://doi.org/10.1002/14651858.CD006205.pub5
- Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature. 2015;517:576-582. doi:https://doi.org/10.1038/nature14129
- Saidak Z, Lailler C, Testelin S. Contribution of genomics to the surgical management and study of oral cancer. Ann Surg Oncol. 2021;28:5842-5854. doi:https://doi.org/10.1245/s10434-021-09904-0
- Dolens E, Dourado M, Almangush A. The impact of histopathological features on the prognosis of oral squamous cell carcinoma: a comprehensive review and meta-analysis. Front Oncol. 2021;11. doi:https://doi.org/10.3389/fonc.2021.784924
- Alix-Panabières C, Marchetti D, Lang J. Liquid biopsy: from concept to clinical application. Sci Rep. 2023;13. doi:https://doi.org/10.1038/s41598-023-48501-x
- Lin L, Chang K, Kao S. Increased plasma circulating cell-free DNA could be a potential marker for oral cancer. Int J Mol Sci. 2018;19. doi:https://doi.org/10.3390/ijms19113303
- Cohen S, Liu M, Aleshin A. Practical recommendations for using ctDNA in clinical decision making. Nature. 2023;619:259-268. doi:https://doi.org/10.1038/s41586-023-06225-y
- Flach S, Howarth K, Hackinger S. Liquid bIOpsy for miNimal rESidual diSease detection in head and neck squamous cell carcinoma (LIONESS) - A personalised circulating tumour DNA analysis in head and neck squamous cell carcinoma. Br J Cancer. 2022;126:1186-1195. doi:https://doi.org/10.1038/s41416-022-01716-7
- Towle R, Dickman C, MacLellan S. Identification of a serum-based microRNA signature that detects recurrent oral squamous cell carcinoma before it is clinically evident. Br J Cancer. 2023;129:1810-1817. doi:https://doi.org/10.1038/s41416-023-02405-9
- Di Cosimo S, Ciniselli C, Pizzamiglio S. End-of-neoadjuvant treatment circulating microRNAs and HER2-positive breast cancer patient prognosis: an exploratory analysis from NeoALTTO. Front Oncol. 2023;12. doi:https://doi.org/10.3389/fonc.2022.1028825
- Goh K, Cheng T, Tham S. Circulating biomarkers for prediction of immunotherapy response in NSCLC. Biomedicines. 2023;11. doi:https://doi.org/10.3390/biomedicines11020508
- Smussi D, Mattavelli D, Paderno A. Revisiting the concept of neoadjuvant and induction therapy in head and neck cancer with the advent of immunotherapy. Cancer Treat Rev. 2023;121. doi:https://doi.org/10.1016/j.ctrv.2023.102644
- Siravegna G, Marsoni S, Siena S. Integrating liquid biopsies into the management of cancer. Nat Rev Clin Oncol. 2017;14:531-548. doi:https://doi.org/10.1038/nrclinonc.2017.14
- Bruschini R, Maffini F, Chiesa F. Oral cancer: changing the aim of the biopsy in the age of precision medicine. A review. Acta Otorhinolaryngol Ital. 2021;41:108-119. doi:https://doi.org/10.14639/0392-100X-N1056
- Kumar P, Gupta S, Das B. Saliva as a potential non-invasive liquid biopsy for early and easy diagnosis/prognosis of head and neck cancer. Transl Oncol. 2024;40. doi:https://doi.org/10.1016/j.tranon.2023.101827
- Sohel M. Extracellular/circulating microRNAs: release mechanisms, functions and challenges. Achievemen Life Sci. 2016;10:175-186. doi:https://doi.org/10.1016/j.als.2016.11.007
- Patel R, Jakymiw A, Yao B. High resolution of microRNA signatures in human whole saliva. Arch Oral Biol. 2011;56:1506-1513. doi:https://doi.org/10.1016/j.archoralbio.2011.05.015
- Git A, Dvinge H, Salmon-Divon M. Systematic comparison of microarray profiling, real-time PCR, and next-generation sequencing technologies for measuring differential microRNA expression. RNA. 2010;16:991-1006. doi:https://doi.org/10.1261/rna.1947110
- Park N, Zhou H, Elashoff D. Salivary microRNA: discovery, characterization, and clinical utility for oral cancer detection. Clin Cancer Res. 2009;15:5473-5477. doi:https://doi.org/10.1158/1078-0432.CCR-09-0736
- Salazar C, Nagadia R, Pandit P. A novel saliva-based microRNA biomarker panel to detect head and neck cancers. Cell Oncol. 2014;37:331-338. doi:https://doi.org/10.1007/s13402-014-0188-2
- Al Rawi N, Elmabrouk N, Abu Kou R. The role of differentially expressed salivary microRNA in oral squamous cell carcinoma. A systematic review. Arch Oral Biol. 2021;125. doi:https://doi.org/10.1016/j.archoralbio.2021.105108
- Kang J, Eun Y, Lee Y. Diagnostic value of salivary miRNA in head and neck squamous cell cancer: systematic review and meta-analysis. Int J Mol Sci. 2021;22. doi:https://doi.org/10.3390/ijms22137026
- Romani C, Salviato E, Paderno A. Genome-wide study of salivary miRNAs identifies miR-423-5p as promising diagnostic and prognostic biomarker in oral squamous cell carcinoma. Theranostics. 2021;11:2987-2999. doi:https://doi.org/10.7150/thno.45157
- Patel A, Patel S, Patel P. Salivary exosomal miRNA-1307-5p predicts disease aggressiveness and poor prognosis in oral squamous cell carcinoma patients. Int J Mol Sci. 2022;23. doi:https://doi.org/10.3390/ij231810639
- Saproo S, Sarkar S, Gautam V. Salivary protein kinase C alpha and novel microRNAs as diagnostic and therapeutic resistance markers for oral squamous cell carcinoma in Indian cohorts. Front Mol Biosci. 2023;10. doi:https://doi.org/10.3389/fmolb.2022.1106963
- Vageli D, Doukas P, Shah R. A novel saliva and serum miRNA panel as a potential useful index for oral cancer and the association of miR-21 with smoking history: a pilot study. Cancer Prev Res (Phila). 2023;16:653-659. doi:https://doi.org/10.1158/1940-6207.CAPR-23-0219
- Cardinali B, Tasso R, Piccioli P. Circulating miRNAs in breast cancer diagnosis and prognosis. Cancers (Basel). 2022;14. doi:https://doi.org/10.3390/cancers14092317
- Sozzi G, Boeri M, Rossi M. Clinical utility of a plasma-based miRNA signature classifier within computed tomography lung cancer screening: a correlative MILD trial study. J Clin Oncol. 2014;32:768-777. doi:https://doi.org/10.1200/JCO.2013.50.4357
- Romani C, Baronchelli M, Assoni C. Stability of circulating miRNA in saliva: the influence of sample associated pre-analytical variables. Clin Chim Acta. 2024;553. doi:https://doi.org/10.1016/j.cca.2023.117702
- Rupaimoole R, Calin G, Lopez-Berestein G. MiRNA deregulation in cancer cells and the tumor microenvironment. Cancer Discov. 2016;6:235-246. doi:https://doi.org/10.1158/2159-8290.CD-15-0893
- Yin V. In situ detection of microRNA expression with RNAscope probes. Methods Mol Biol. 2018;1649:197-208. doi:https://doi.org/10.1007/978-1-4939-7213-5_13
- Livak K, Schmittgen T. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402-408. doi:https://doi.org/10.1006/meth.2001.1262
- Sequeira J, Constâncio V, Salta S. LiKidMiRs: a ddPCR-based panel of 4 circulating miRNAs for detection of renal cell carcinoma. Cancers. 2022;14. doi:https://doi.org/10.3390/cancers14040858
- Hindson C, Chevillet J, Briggs H. Absolute quantification by droplet digital PCR versus analog real-time PCR. Nat Methods. 2013;10:1003-1005. doi:https://doi.org/10.1038/nmeth.2633
- Ferracin M, Lupini L, Salamon I. Absolute quantification of cell-free microRNAs in cancer patients. Oncotarget. 2015;6:14545-14555. doi:https://doi.org/10.18632/oncotarget.3859
- Castagnola M, Scarano E, Passali G. Salivary biomarkers and proteomics: future diagnostic and clinical utilities. Acta Otorhinolaryngol Ital. 2017;37:94-101. doi:https://doi.org/10.14639/0392-100X-1598
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2024 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1225 times
- PDF downloaded - 234 times



