Head and neck
Vol. 45: Issue 6 - December 2025
Prognosis of patients with carotid blowout syndrome in the era of endovascular interventions
Abstract
Objective. To analyse the prognosis of carotid blowout syndrome (CBS) after endovascular interventions in patients with head and neck cancer.
Methods. We conducted a retrospective study at a tertiary centre (2000-2019), including demographics, medical history, treatment details, and outcomes of CBS.
Results. Among 44 patients with CBS (32 males, 12 females; mean age 65 ± 14 years), squamous cell carcinoma histotype and laryngeal localisation were most common, with 84% having advancedstaged disease. Significant risk factors included prior surgery (70%), neck dissection (48%), radiation (55%), and chemotherapy (66%). Pharyngocutaneous fistula and tracheostomy were present in 32% and 57% of cases, respectively. Radiological findings showed threatened bleeding (62%), sentinel bleeding (11%), and acute rupture (27%). Endovascular treatment achieved haemostasis in 95% of cases, with an 11% rate of acute ischaemic complications. Six-month survival was 28%, with 66% of deaths due to disease progression. Recurrent bleeding occurred in 16% of cases.
Conclusions. CBS is a severe complication with a high risk of rebleeding. Endovascular interventions effectively manage bleeding with low rates of complication.
Introduction
Carotid blowout syndrome (CBS) is the rupture of the carotid arteries or one of their major branches 2. It represents a devastating complication of head and neck (H&N) cancer and its treatments 3. The reported incidence of this complication following radical neck dissection is 4.3%, while it rises to 17% after reirradiation for head and neck cancer 4. CBS can be categorised into three types based on the threat of massive bleeding: threatened, impending, and acute (Type I-III) 5. Diagnosis of CBS can be achieved through clinical examination (e.g., exposed, dissected carotid artery within an open wound), radiologic images (e.g., air surrounding vessels, adjacent necrosis, or abscess with fistula), or vascular imaging studies (demonstrating areas of arterial wall disruption, aneurysm/pseudoaneurysm) 6. Without intervention, this phase may lead to bleeding. Impending CBS (Type II or sentinel haemorrhage) refers to transient haemorrhage resolving spontaneously or with mild intervention (packing or pressure). Acute CBS (Type III) involves bleeding necessitating surgical/endovascular approaches, and it often turns rapidly lethal, particularly in outpatient settings 7.
CBS tends to occur in patients with persistent or recurrent H&N cancer 3, those with a history of neck irradiation 4, wound complications, and pharyngocutaneous fistula 8. Emergency surgical management of CBS is often technically challenging, especially in previously irradiated necks, and is associated with neurological morbidity and mortality rates of 40% and 60%, respectively 8. Since the introduction of endovascular treatment for CBS, the morbidity rate has decreased to 0-8%, and the mortality rate is very low 9. However, complications of endovascular treatment include delayed cerebral ischaemic complications (15-20% of cases) arising from incomplete perfusion of the circle of Willis, thromboembolism from acutely occluded carotid arteries, and delayed collateral failure 10. Our study describes our experience with endovascular intervention in patients with H&N cancer and CBS, their prognoses, and predictors for morbidity and survival. This study hypothesises that advanced endovascular interventions enhance survival rates and outcomes in patients with CBS. By focusing on the effectiveness of these interventions, the research addresses a gap in the current literature that lacks a comprehensive analysis of long-term outcomes following endovascular treatments for CBS.
Materials and methods
Following IRB approval (RMC 0731-21), we conducted a retrospective study at the Department of Otorhinolaryngology and Head and Neck Cancer in Rabin Medical Center – a referral, university-affiliated medical centre – between 2000 and 2019. All patients with a history of H&N cancer and CBS were eligible for the study, while exclusion criteria included patients with bleeding unrelated to H&N cancer. We reviewed medical records and extracted information on demographics, medical history, time of H&N cancer diagnosis, radiological scans, surgical and oncological treatments, CBS diagnosis time, surgical and neurovascular interventions, and long-term follow-up and prognosis.
In this study, endovascular interventions included both embolisation and stenting, tailored to the anatomical and clinical requirements of each case. Stents were primarily used to scaffold and stabilise damaged arterial segments, particularly where the structural integrity of the vessel wall was compromised. The procedure involved placing a stent across the affected artery segment to exclude the pseudoaneurysm or disrupted area while maintaining arterial patency. Concurrently, embolisation was performed using coils or other embolic materials deployed within the stented segment to promote thrombosis and seal off the source of bleeding. This combination aimed to reinforce the arterial wall, prevent re-rupture, and ensure continuous blood flow, especially in regions critical for cerebral perfusion. The choice of stent-assisted embolisation over standalone embolisation was driven by factors such as the extent of arterial damage, risk of haemodynamic instability, and previous unsuccessful interventions, ensuring a customised approach to managing CBS in H&N cancer patients.
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software version 25.0. Mean values and standard deviations represented continuous variables. Categorical variables were analysed using the chi-squared test, and associations between categorical variables were assessed using the Spearman correlation coefficient. A significance level of p < 0.05 was employed for all tests.
Results
Demographics and clinical characteristics
We identified 44 patients with a history of H&N cancer and CBS, consisting of 32 males and 12 females (male-to-female ratio: 2.7:1). The mean age at CBS diagnosis was 65 ± 14 years. Squamous cell carcinoma (SCC; n = 36, 82%) and papillary thyroid carcinoma (n = 5, 11%) were the most prevalent histologies, with the larynx being the most frequently affected primary tumour site (34%, n = 15). At the initial cancer diagnosis, 84% (n = 37) of the patients were diagnosed with advanced-staged disease (Stage III-IV), while the remaining 16% (n = 7) were initially diagnosed at an early stage (Stage I-II). Notably, by the time of the CBS event, all patients, including those initially diagnosed at an early stage, had progressed to advanced-staged disease (Tab. I).
Risk factors
Surgical intervention on the primary site had been performed in 70% of cases (n = 31), including neck dissection in 48% of patients (n = 21). Radiation therapy had been administered to 55% of patients (n = 24), targeting the primary tumour site and associated lymphatic regions in the H&N area. Among these patients, 14 (32%) underwent multiple irradiation courses primarily to manage persistent or recurrent H&N cancer. The average total radiation exposure was 103 ± 53 Gy.
Chemotherapy was administered to 66% of patients (n = 29). In all, 82% of those received chemotherapy (n = 24) as adjuvant treatment together with radiation therapy, while the remaining 18% (n = 5) received systemic chemotherapy for recurrent or metastatic H&N SCC when neither surgical nor localised therapeutic options were viable.
Pharyngocutaneous fistulae were observed in 32% of patients (n = 14), and tracheostomies were performed in 57% (n = 25) due to compromised airway integrity or persistent disease burden. Additionally, 93% of patients (n = 41) exhibited elevated inflammatory markers, such as leukocytosis and C-reactive protein, at the time of CBS (Tab. I).
Carotid blowout events
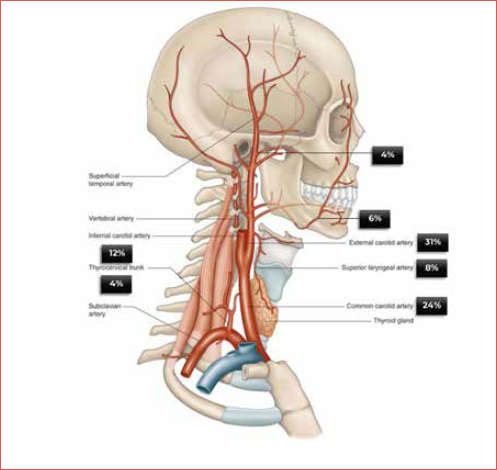
A total of 51 CBS events occurred in 44 patients. Threatened bleeding occurred in 62% of cases, sentinel bleeding in 11%, and acute rupture with profuse uncontrolled bleeding in 7 patients (16%) (Tab. II). The most common sources of bleeding were the external carotid and common carotid arteries (Cover figure).
Neurovascular intervention
Neurovascular intervention was the preferred treatment in 92% (n = 47) of events. Among the 67% (n = 34) treated with an embolisation procedure, 26% (n = 13) included insertion of a stent for revascularization. Figures 1 and 2 describe two specific occurrences of an imminent carotid blowout and the neurovascular intervention adopted.
Outcomes
Successful haemostasis was achieved in 95% of cases. One patient required surgical intervention with ligation of the common carotid artery on post-procedure day 7 following stenting due to rebleeding. Another patient received surgical ligation of the common carotid artery as a primary intervention. Unfortunately, two patients succumbed to massive uncontrolled bleeding before they could receive neurovascular intervention. Neurological complications were observed in 5 patients (11%). Specifically, ischaemic strokes resulting in hemiparesis occurred in both patients who underwent surgical ligation and one patient who had angiographic closure of the artery. One patient who received a stent experienced a transient ischaemic attack, resolving within 24 hours.
Eighty-four percent of patients (n = 37) survived the initial bleeding event. The 6-month survival rate was 66%, with 18% of patients (n = 8) still alive at the end of the follow-up period. Seven patients suffered subsequent bleeding episodes, and all succumbed to rebleeding, underscoring the critical nature of ongoing monitoring and intervention (Fig. 3).
Sub-population analysis
REBLEEDING
Rebleeding occurred in 16% (n = 7) of patients. No significant differences were found in demographics, clinical features, or treatment options between patients with recurrent CBS events and those with a single event. Additionally, no statistically significant difference was observed between radiation dose and rebleeding (p = 0.64). However, an association was noted between death from bleeding and cervical fistula after surgery or neck dissection, with correlation coefficients of 0.29 (p = 0.04) and 0.39 (p = 0.0084), respectively. Notably, the overall survival for patients with recurrent bleeding was 0% after two months, compared to 60% for those with a single CBS event (log-rank p value = 0.001) (Fig. 4).
STENT VS OCCLUSION
A comparison of treatment arms revealed significant differences between the 13 patients treated with endovascular stents and the 34 patients treated with occlusion of the culprit vessel. A higher proportion of patients with tracheostomy was observed in the stent group (85% vs 50%, p = 0.05). Patients with occlusion of the culprit vessel bled primarily from the external carotid artery (35% vs 15%) and superior thyroid artery (12% vs 0%) (p = 0.01). Nevertheless, no difference in overall survival was observed between groups.
6-MONTH SURVIVAL
Evaluation of patient and clinical characteristics and treatment modalities for CBS bleeding sites did not reveal differences between patients who survived less than 6 months and those who survived longer than 6 months after the CBS event, except for a recurrent event of carotid blowout that was linked to 100% mortality after two months.
Discussion
This manuscript presents the experience of a single tertiary centre involving 51 CBS events among 44 patients, showing a high success rate for endovascular interventions, with no advantage for one modality over the other (embolization vs stenting). Furthermore, even with a multidisciplinary approach involving H&N surgeons, interventional and diagnostic radiologist rebleeding events have a grave prognosis with 100% 2-month mortality.
CBS is one of the most devastating complications of H&N cancers and their treatments 11. Clinical characteristics of patients with this catastrophic complication typically include advanced-staged tumours, radiation treatment, and local recurrence 12, as demonstrated in our study. Higher radiation doses, especially reirradiation 13, and induction or concurrent chemotherapy 1 have been associated with a greater CBS incidence, consistent with our findings. Lu et al. 14 and Mattavelli et al. 15 reported that the neutrophil-to-lymphocyte ratio negatively predicted overall survival. Inflammatory markers reflect systemic inflammation and physiologic stress severity 16,17. Therefore, in patients with systemic stress/inflammation and local endothelial injury, these markers indicate endovascular injury degree and disease severity 18. Our study supports that patients suffering from CBS had elevated inflammatory markers before the event.
In a comprehensive meta-analysis by Bond et al. 19, an extensive examination of CBS cases was undertaken. The analysis discerned distinct manifestations within a cohort of 559 patients presenting with CBS. Specifically, 287 patients (51%) exhibited acute bleeding, while 272 (49%) presented with threatened or impending bleeding. These classifications provide valuable insights into the heterogeneity of CBS presentations among afflicted individuals. The predominant sites of vascular involvement in CBS-induced bleeding were consistently reported in previous studies, affirming the prominence of the external carotid artery and common carotid artery as the most frequently affected vessels 20. In our institutional study, the presentation of CBS cases showcased a noteworthy pattern. A substantial majority, encompassing 62% of patients, presented with threatened bleeding, whereas 27% presented with the gravest form of the condition – acute rupture, characterised by profuse haemorrhage. This dichotomy in CBS presentation underscores the imperative nature of early detection and the critical role played by a high index of suspicion within our institution’s clinical practice. The compelling correlation between early diagnosis and enhanced prognostic outcomes in CBS cannot be understated. Previous investigations have demonstrated that prompt identification and management of threatened CBS confer significantly improved prognosis and extended survival rates compared to cases where intervention is delayed until overt carotid bleeding occurs 14.
Endovascular treatment for CBS has shown high success rates ranging from 95% to 100% 19. Similar to our study, no differences in overall survival were noted between embolisation and stenting procedures 21. However, our study reveals two noteworthy findings. First, a higher proportion of tracheostomy patients was observed in the stent group. This could be attributed to a possibly higher rebleeding rate with stents than occlusion 22. However, patients with tracheostomy likely had better airway control and direct pressure, which can manage acute rebleeding while benefiting from reduced stroke rates offered by stents compared to occlusion. Second, stent placement predominantly involved the common carotid artery (CCA), internal carotid artery (ICA), or external carotid artery (ECA), with the majority in the CCA. This aligns with concerns about occluding the carotid artery system, which could risk neurovascular compromise. A balloon occlusion test could help decide intraoperatively whether a stent or angiographic occlusion should be pursued.
Warren et al. and Yamazaki et al. reported immediate or delayed ischaemia in 15-20% of CBS patients treated with permanent balloon occlusion 2,9. In our study, only 11% experienced neurological complications. One patient had a transient ischaemic attack, which resolved within 24 hours, and three patients had ischaemic strokes resulting in permanent hemiparesis – all underwent devascularisation procedures.
In a meta-analysis, the incidence of recurrent bleeding was reported as 44% by Lu et al. 14 and 27% by Bond et al. 19. In our study, rebleeding occurred in 16% of patients, and no specific characteristics were found distinguishing between those with single CBS events and recurrent events. Associations between demographics, disease-related factors, and treatment-related aspects differed between the two groups. Luo et al. 23 reported recurrent CBS in 14% of cases and up to 47% using covered stents, with the carotid bulb and main trunk of the external carotid artery being common recurrent CBS locations, consistent with our findings. Recurrent bleeding resulted from disease progression in seven patients, extravasation of a stent through the common carotid artery in one patient, and infected pharyngocutaneous fistula in two patients. Previous studies show that the death from recurrent bleeding is estimated to be 50% in the acute event 3. However, our study is the first to address a more extended follow-up for recurrent bleeding than only the immediate period. Our study shows a 100% mortality within two months, suggesting that the grave prognosis might suggest a need for an informed shared decision-making process with these patients and their families, possibly offering a more conservative treatment focusing on pain control, palliation, and addressing patients’ and caregivers’ needs with a comprehensive expectation discussion.
As previous studies have highlighted, CBS represents a devastating complication in already debilitated patients with advanced-staged H&N SCC, some of whom have recurrent tumours and are treated using various modalities including radiation, chemotherapy, surgery, lymph node dissection, and even re-irradiation with high cumulative radiation doses. Our study demonstrates that the 6-month overall survival rate is 28%. Furthermore, while survival at two months after a single CBS event was 60%, it was 0% for patients with recurrent CBS events. Importantly, no overall survival difference was observed between embolisation and stenting procedures. However, we identified an association between death from bleeding and both cervical fistula and neck dissection.
Finally, several preventive measures can reduce the risk of CBS. Modern irradiation techniques, especially for reirradiation (e.g., intensity-modulated radiotherapy, hypofractionation, and stereotactic irradiation with carotid dose constraints), can lower its risk 24. Active measures include endovascular interventions with various stents 25 and surgical approaches using local, regional, free flaps, or interposition of the sternocleidomastoid. In light of our findings, where pharyngocutaneous fistula was significantly associated with CBS, with 32% of patients (14 of 44) experiencing this complication, it is crucial to invest any effort needed in preventing and managing such fistulas to mitigate the risk of CBS. The incidence of pharyngocutaneous fistula following total laryngectomy has been reported to range from 21.3% to 23% in various studies 26. The liberal use of free or pedicled flaps in reconstructive surgery can play a pivotal role in this regard. These surgical strategies not only facilitate the closure and healing of potential or existing fistulas but also contribute to reinforcing the structural integrity of the neck tissues, which can be compromised in head and neck cancer treatments 27. By prioritising early intervention and employing advanced reconstructive techniques, the risk of developing CBS can be significantly reduced, thereby improving the overall prognosis for patients. Given the severe outcomes associated with CBS, as evidenced by the high rate of recurrence and mortality in our series, where recurrent bleeding was observed in 16% of cases and 6-month survival was only 28%, preventive measures, including meticulous surgical planning and execution, should be emphasised as a critical component of comprehensive care for H&N cancer patients. Considering the acute and devastating nature of CBS, which carries neurologic morbidity and mortality rates of 40% and 60% respectively, we advocate for an individually tailored management approach that involves a multidisciplinary team including a head and neck surgeon, a head and neck-oriented interventional radiologist, and a radiologist.
While our study provides valuable insights into the management of CBS in patients with H&N cancers, several limitations must be acknowledged. First, our retrospective study can introduce inherent biases and limitations. Second, the study was conducted at a single tertiary centre, which might limit the generalisability of our results to broader populations. Additionally, due to the rarity of CBS and the heterogeneity of H&N tumours, we did not create comparative rates, which may limit the depth of our analyses. Third, although we reported short-term outcomes and survival rates, our study has limited long-term follow-up and a small sample size of 44 patients, underscoring this cohort’s notably high mortality rate.
Conclusions
CBS represents a significant complication in patients with H&N cancer, where endovascular treatment has proven to be a highly effective method for controlling bleeding. This study has demonstrated that endovascular techniques, specifically stenting and embolisation, are critical in managing CBS with a relatively low rate of complications.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
NT, YR: conception and design; GB: administrative support; AE: provision of study materials or patients; NT, YR, AE: collection and assembly of data, data analysis and interpretation. All authors: manuscript writing, final approval of manuscript.
Ethical consideration
This study was approved by the Institutional Ethics Committee (Rabin Medical Center) (approval number/protocol number IRB-073-21).
The research was conducted ethically, with all study procedures being performed in accordance with the requirements of the World Medical Association’s Declaration of Helsinki. Written informed consent was obtained from each participant/patient for study participation and data publication.
History
Received: December 31, 2024
Accepted: June 18, 2025
Figures and tables
Figure 1. A sagittal CT angiography of a 62-year-old male with advanced laryngeal SCC post-CRT showed a pseudoaneurysm in the left common carotid artery near the stoma site. The image highlights the coil embolisation targeting the left ECA to mitigate the risk of rupture.
Figure 2. Shows sagittal CT and CTA images of a 64-year-old male revealing an aneurysm in the left internal carotid artery with peristomal bleeding. Post-treatment images demonstrate the successful placement of a stent, which bypasses the affected ICA segment, controlling the source of hemorrhage.
Figure 3. Kaplan-Meier survival curve depicting the time from bleeding to death in months for patients with carotid blowout syndrome. The number of patients at risk at each time point is shown below the curve: 44 at start, 30 at 2 months, 20 at 4 months, and 10 at 6 months. Patients who are censored are marked with a ‘+’.
Figure 4. Kaplan-Meier curve for the rebleeding group. Two-month overall survival rates are 60% for non-bleeding versus 0% for bleeding groups, with a log-rank p value of 0.001.
| Clinical characteristics | n = 44 |
|---|---|
| Demographics | |
| Male gender, n (%) | 32 (73) |
| Age at diagnosis, years (mean ± sd) | 65 ± 14 |
| Pathology | |
| SCC + adenoid cystic | 36 (82) |
| PTC + anaplastic | 5 (11) |
| Other | 3 (7) |
| Tumour site | |
| Nasopharynx | 6 (14) |
| Oral cavity | 8 (18) |
| Larynx and hypopharynx | 19 (43) |
| Thyroid cancer | 5 (11) |
| Other sites | 6 (14) |
| Staging | |
| Stage I | 4 (9) |
| Stage III | 8 (18) |
| Stage IV | 29 (66) |
| Total radiation dose (Gy) (mean ± sd) | 103 ± 53 |
| Courses of radiation therapy | |
| 1 | 24 (55) |
| 2 | 14 (32) |
| 3 or more | 4 (10) |
| Adjuvant chemotherapy | 29 (66) |
| Surgery | 31 (71) |
| Neck dissection | 21 (48) |
| Cervical fistula after surgery | 14 (32) |
| Positive inflammation markers | 41 (93) |
| Tracheostomy | 25 (57) |
| SCC: squamous cell carcinoma; PTC: papillary thyroid carcinoma. Percentages may not sum to 100 due to rounding. | |
| Total events of CBS | Threatened | Overt bleeding | Occlusion | ||
|---|---|---|---|---|---|
| n = 44 | n = 7 | n = 34 | |||
| Bleeding sites | |||||
| CCA | 12 (28) | 0 (0) | 5 (15) | ||
| ICA | 6 (14) | 0 (0) | 2 (6) | ||
| ECA | 11 (26) | 5 (72) | 12 (35) | ||
| Superior thyroid artery | 4 (9) | 0 (0) | 4 (12) | 0.062 | |
| Facial artery | 3 (7) | 0 (0) | 3 (9) | ||
| Multiple branches of ECA | 5 (12) | 0 (0) | 5 (15) | ||
| Internal maxillary artery | 1 (2) | 1 (14) | 2 (6) | ||
| Thyrocervical trunk | 1 (2) | 1 (14) | 1 (3) | ||
| Type of angiography | |||||
| Stent | 12 (28) | 1 (25) | |||
| Occlusion | 31 (72) | 3 (75) | 1 | ||
| CCA: common carotid artery; ICA: internal carotid artery; ECA: external carotid artery. Percentages may not sum to 100 due to rounding. The value 0.062 relates to the p value for statistical significance in the difference of occurrences across bleeding sites. | |||||
References
- Cheng C, ed. Handbook of Vascular Motion. Elsevier; 2019.
- Yamazaki H, Ogita M, Kodani N. Frequency, outcome and prognostic factors of carotid blowout syndrome after hypofractionated re-irradiation of head and neck cancer using CyberKnife: a multi-institutional study. Radiother Oncol. 2013;107:305-309. doi:https://doi.org/10.1016/j.radonc.2013.01.032
- Suárez C, Fernández-Alvarez V, Hamoir M. Carotid blowout syndrome: modern trends in management. Cancer Manag Res. 2018;10:5617-5628. doi:https://doi.org/10.2147/CMAR.S168483
- McDonald M, Moore M, Johnstone P. Risk of carotid blowout after reirradiation of the head and neck: a systematic review. Int J Radiat Oncol Biol Phys. 2012;82:1083-1089. doi:https://doi.org/10.1016/j.jrobp.2011.09.022
- Silverman D, Parikh A, Liu K. Predictors of survival following carotid blowout syndrome. Oral Oncol. 2022;125. doi:https://doi.org/10.1016/j.oraloncology.2022.105723
- Chen C, Lin Y, Chen Y. Air-containing necrosis as the imaging predictor for imminent carotid blowout in patients with head and neck cancer. J Formos Med Assoc. 2022;121:1266-1272. doi:https://doi.org/10.1016/j.jfma.2021.09.017
- Yazici G, Sanlı T, Cengiz M. A simple strategy to decrease fatal carotid blowout syndrome after stereotactic body reirradiaton for recurrent head and neck cancers. Radiat Oncol. 2013;8. doi:https://doi.org/10.1186/1748-717X-8-242
- Gleysteen J, Clayburgh D, Cohen J. Management of carotid blowout from radiation necrosis. Otolaryngol Clin North Am. 2016;49:829-839. doi:https://doi.org/10.1016/j.otc.2016.03.006
- Warren F, Cohen J, Nesbit G. Management of carotid ‘blowout’ with endovascular stent grafts. Laryngoscope. 2002;112:428-433. doi:https://doi.org/10.1097/00005537-200202000-00018
- Weinberg J, Sweid A, Joffe D. Carotid blowout management in the endovascular era. World Neurosurg. 2020;141:E1010-E1016. doi:https://doi.org/10.1016/j.wneu.2020.01.151
- Powitzky R, Vasan N, Krempl G. Carotid blowout in patients with head and neck cancer. Ann Otol Rhinol Laryngol. 2010;119:476-484. doi:https://doi.org/10.1177/0003489410366843
- Jacobi C, Gahleitner C, Bier H. Chemoradiation and local recurrence of head and neck squamous cell carcinoma and the risk of carotid artery blowout. Head Neck. 2019;41:3073-3079. doi:https://doi.org/10.1002/hed.25667
- Yamazaki H, Ogita M, Himei K. Carotid blowout syndrome in pharyngeal cancer patients treated by hypofractionated stereotactic re-irradiation using CyberKnife: a multi-institutional matched-cohort analysis. Radiother Oncol. 2015;115:67-71. doi:https://doi.org/10.1016/j.radonc.2015.01.033
- Lu H, Chen K, Chen M. Predisposing factors, management, and prognostic evaluation of acute carotid blowout syndrome. J Vasc Surg. 2013;58:1226-1235. doi:https://doi.org/10.1016/j.jvs.2013.03.054
- Mattavelli D, Lombardi D, Missale F. Prognostic nomograms in oral squamous cell carcinoma: the negative impact of low neutrophil to lymphocyte ratio. Front Oncol. 2019;9. doi:https://doi.org/10.3389/fonc.2019.00339
- Kantola T, Klintrup K, Väyrynen J. Stage-dependent alterations of the serum cytokine pattern in colorectal carcinoma. Br J Cancer. 2012;107:1729-1736. doi:https://doi.org/10.1038/bjc.2012.368
- Ueda T, Aoyama-Ishikawa M, Nakao A. A simple scoring system based on neutrophil count in sepsis patients. Med Hypotheses. 2014;82:382-386. doi:https://doi.org/10.1016/j.mehy.2013.12.015
- de Jager C, Wever P, Gemen E. The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS One. 2012;7. doi:https://doi.org/10.1371/journal.pone.0031622
- Bond K, Brinjikji W, Murad M. Endovascular treatment of carotid blowout syndrome. J Vasc Surg. 2017;65:883-888. doi:https://doi.org/10.1016/j.jvs.2016.08.073
- Dionisi F, Fiorica F, D’Angelo E. Organs at risk’s tolerance and dose limits for head and neck cancer re-irradiation: a literature review. Oral Oncol. 2019;98:35-47. doi:https://doi.org/10.1016/j.oraloncology.2019.04.006
- Simizu Y. Endovascular treatment of carotid blowout syndrome. J Stroke Cerebrovasc Dis. 2021;30. doi:https://doi.org/10.1016/j.jstrokecerebrovasdis.2021
- Wong D, Donaldson C, Lai L. Safety and effectiveness of endovascular embolization or stent-graft reconstruction for treatment of acute carotid blowout syndrome in patients with head and neck cancer: case series and systematic review of observational studies. Head Neck. 2018;40:846-854. doi:https://doi.org/10.1002/hed.25487
- Luo C, Lee C, Chang F. Risk factors of recurrent carotid blowout syndrome and strategy of endovascular management. J Chin Med Assoc. 2022;85:109-113. doi:https://doi.org/10.1016/j.jcma.2021.09.018
- Hung H, Chan O, Mak C. Dosimetric comparison of intensity modulated radiotherapy and intensity modulated proton therapy in the treatment of recurrent nasopharyngeal carcinoma. Med Dosim. 2022;47:14-19. doi:https://doi.org/10.1016/J.MEDDOS.2021.07.002
- Gaynor B, Haussen D, Ambekar S. Covered stents for the prevention and treatment of carotid blowout syndrome. Neurosurgery. 2015;77:164-167. doi:https://doi.org/10.1227/NEU.0000000000000702
- Dedivitis R, Aires F, Cernea C. Pharyngocutaneous fistula after total laryngectomy: systematic review of risk factors. Head Neck. 2015;37:1691-1697. doi:https://doi.org/10.1002/hed.23804
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 653 times
- PDF downloaded - 154 times



