Head and neck
Vol. 45: 111TH CONGRESS SIOECHCF - OFFICIAL REPORT 2025
The impact of resection margins in hypopharyngeal surgery: a systematic review and meta-analysis
Abstract
Objective. Hypopharyngeal squamous cell carcinoma is an aggressive malignancy with poor prognosis due to frequently late-stage presentation and intrinsic anatomical complexity. Surgery remains a key treatment, and resection margins are crucial for local control and survival. However, achieving adequate margins is challenging due to submucosal tumour spread and common “skip lesions”. This systematic review examines the impact of positive and close margins on oncological outcomes and their role in treatment planning.
Methods. Following PRISMA guidelines, we included studies on adult hypopharyngeal cancer patients undergoing surgical treatment, including transoral laser microsurgery, transoral robotic surgery and open resections. The primary outcome was overall survival (OS); secondary outcomes included disease-free survival (DFS), disease-specific survival (DSS), and local control. A systematic search of PubMed, EMBASE, and Cochrane databases from 2000 to 2024 was conducted, with eligible studies screened based on strict inclusion criteria. Random-effect meta-analysis was used to estimate the pooled hazard ratio (HR) and relative 95% confidence interval (CI).
Results. From an initial pool of 2,681 articles, 157 full-text studies were reviewed, and 7 met inclusion criteria. Data on 619 patients (mean age, 60.9 years) were analysed, all from retrospective studies. Among these, 17% received neoadjuvant chemotherapy, while 94% underwent adjuvant treatment due to positive margins or other adverse features. A meta-analysis found no statistically significant impact of positive or close margins on OS, DSS, or DFS when compared to negative ones. OS had an HR of 1.78 (95%CI: 0.79- 4.04, p = 0.17), DFS HR 1.43 (95%CI: 0.82-2.49, p = 0.21), and DSS HR 1.31 (95%CI: 0.42-4.05, p = 0.42).
Conclusions. This review underscores the challenges of achieving optimal margins in hypopharyngeal cancer surgery. While positive and close margins increase the risk of recurrence, their impact on survival remains unclear, emphasising the need for standardised margin assessment and tailored treatment strategies. The significant submucosal spread and presence of skip lesions necessitates a multidisciplinary approach. Future research should refine surgical techniques, improve intraoperative margin assessment, and optimise adjuvant therapy protocols to enhance oncologic outcomes.
Introduction
Hypopharyngeal carcinomas pose a significant challenge in the oncological landscape of the upper aerodigestive tract due to their biological aggressiveness, relative rarity, and anatomical complexity of the region 1. Although these tumours account for a small proportion of head and neck cancers in the Western population, their incidence varies considerably worldwide, with a higher prevalence observed in certain regions, such as Japan (20%) 2. Late diagnosis and a tendency to be treated at advanced stages contribute to a generally poor prognosis, with 5-year overall survival (OS) rates rarely exceeding 35% 3.
Clinical management of these tumours is further complicated by a high incidence of positive regional lymph nodes (60%) and distant metastases (10-30%), both of which significantly exceed the rates usually observed in other head and neck squamous cell carcinomas 4. Regardless of their morphological pattern, these tumours often exhibit submucosal growth extending up to 8 mm within the piriform sinus and post-cricoid region 5. This characteristic makes both preoperative assessment – despite the use of advanced imaging modalities such as MRI – and intraoperative detection particularly challenging in ensuring adequate surgical resections 6.
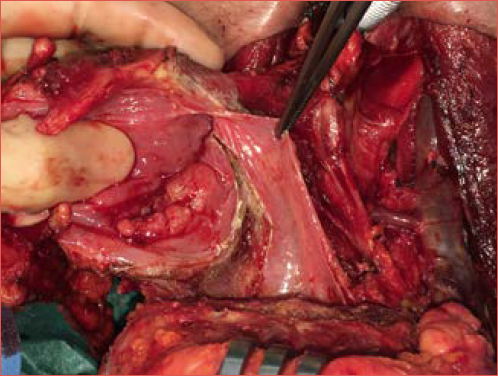
A critical aspect of the surgical management of hypopharyngeal carcinomas is the assessment of its resection margins (Cover figure). The surgical approach varies depending on tumour stage and anatomical characteristics. For early-stage tumours, transoral techniques, such as transoral laser microsurgery (TOLMS) and transoral robotic surgery (TORS), have expanded the indications for conservative treatment by minimising surgical trauma and improving functional outcomes in selected cases. However, these techniques sometimes fall short in achieving adequate three-dimensional margins. For locally advanced tumours, radical surgery – typically total pharyngolaryngectomy (TPL) – remains the standard treatment, often combined with adjuvant radiotherapy or chemoradiotherapy.
According to the Royal College of Pathologists (RCP) guidelines, resection margins are categorised as clear (> 5 mm), close (1-5 mm), or positive (< 1 mm). However, achieving margins > 5 mm in hypopharyngeal surgery is often extremely challenging, even with open neck approaches, due to the complex anatomy of this region 7. Tumours in this area can grow in multiple directions, infiltrating surrounding structures or spreading along the cranio-caudal axis of the organ 8. This necessitates a delicate balance between oncological radicality and preservation of healthy tissues to ensure functional recovery and maintain an acceptable quality of life.
The presence of “skip lesions” – microtumour foci seemingly detached from the main tumour mass – further complicates the achievement of adequate margins and the accuracy of postoperative pathological assessment 9. Moreover, the frequent occurrence of lympho-vascular invasion (LVI), perineural invasion (PNI) and the high incidence of regional lymph nodes metastases highlight the need for integrated multidisciplinary management 10.
The clinical implications of positive or close resection margins in upper aerodigestive tract surgery have been extensively investigated. Several studies have demonstrated that positive margins (< 1 mm) are associated with a significantly increased risk of local and locoregional recurrence, as well as the need for adjuvant therapies 11,12. However, the prognostic significance of resection margins in hypopharyngeal carcinomas remains controversial. On one hand, adjuvant radiotherapy – frequently employed to address adverse prognostic factors such as positive margins, PNI, and LVI – can obscure the true negative impact of margins on survival. On the other hand, clinical evidence supporting the efficacy of margins > 5 mm in improving OS or disease-free survival (DFS) remains limited and, at times, contradictory.
This systematic review aims to analyse the impact of positive margins in hypopharyngeal surgery focusing on oncological outcomes and multimodal therapy selection. Specifically, it will explore the role of positive and close margins in the context of adjuvant treatments and their prognostic significance in terms of locoregional control and survival. The goal is to provide a clearer and more comprehensive understanding of the challenges and opportunities in the management of hypopharyngeal carcinomas, offering insights to improve integrated and personalised therapeutic strategies.
Materials and methods
This study strictly followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 13. Ethics committee approval or informed consent was not required, as all data were obtained from publicly available literature.
The inclusion criteria for study selection were based on the PICOS framework: Population (P), adults with squamous cell carcinoma of the hypopharynx undergone open neck or transoral surgery (by CO2 laser [TOLMS] or robot [TORS]); Intervention (I), positive margins; Comparator (C), negative margins; Outcome (O), OS as primary outcome, local control (LC), DFS and disease-specific survival (DSS) as secondary outcomes; Study design (S), retrospective. A systematic search was conducted for articles published between January 2000 and August 2024 in the PubMed, EMBASE, and Cochrane Library databases using the following combined search query: (“hypopharynx” OR “hypopharyngeal” OR “piriform sinus” OR “pharynx”) AND (“cancer” OR “carcinoma” OR “tumour” OR “neoplasm”) AND (“TLM” OR “TORS” OR “TOLMS” OR “TOLM” OR “transoral surgery” OR “microlaryngoscopy” OR “laser” OR “total laryngectomy” OR “hypopharyngectomy” OR “pharyngolaryngectomy” OR “laryngopharyngectomy” OR “pharyngolaryngoesophagectomy” OR “laryngoesophagectomy”) NOT (“thyroid” OR “salivary gland” OR “oral cavity” OR “oropharyngeal”).
The full texts of relevant studies were reviewed independently in double for final selection. References from all included papers were screened to identify any additional eligible study. The most recent publication was selected if multiple manuscripts from the same research group or centre described overlapping case series.
Eligibility assessment
Two pairs of authors (FP, CG and GF, CA) independently reviewed the studies identified in the initial search across the 3 databases. Articles were included only if both reviewers agreed. In case of disagreement, the full text was examined and, if uncertainty persisted, consultation with 2 expert authors (GS, EC) was sought.
Following our PICOS framework, the study focused on patients with squamous cell carcinoma of the hypopharynx who underwent open or transoral surgery (TOLMS and TORS) as primary treatment. The inclusion criteria were as follows:
- squamous cell carcinoma of the hypopharynx confirmed by histopathological examination;
- staging according to the American Joint Committee on Cancer (AJCC) 14;
- patients surgically treated with open surgery or transoral surgery, with or without neck dissection;
- no prior curative treatment;
- margins reported as clear/close/positive;
- margin status correlated with at least one of the following oncological outcomes: LC, DSS, DFS or OS.
The exclusion criteria were:
- duplicate articles;
- book chapters;
- case reports;
- poster presentations;
- articles analysing head and neck tumours other than squamous cell carcinoma or squamous cell carcinomas originating from sites other than the hypopharynx;
- articles not written in English.
OS was defined as the time from surgery to death or the last follow-up. LC was defined as the time from surgery to local recurrence or the last follow-up. DSS was defined as the time from surgery to cancer-related death or the last follow-up, and DFS was the time until local, nodal or distant recurrence or the last follow-up.
Data extraction
The data extracted included the following: first author, year of publication, patient recruitment method, country, number of patients, age, gender, neck treatment, adjuvant treatment, TNM stage (AJCC 6th, 7th, or 8th Edition), level of evidence (LOE) 15, margin status (positive, negative, close), adjusted hazard ratio (aHR, based on margin status as a categorical variable distinguished into negative, close or positive), non-adjusted hazard ratio (naHR, for LC, OS, DSS, DFS), and follow-up duration. Studies without an aHR were excluded from the quantitative synthesis but included in the qualitative evaluation.
Study quality assessment
The risk of bias was independently assessed by each reviewer according to the Reporting Recommendations for Tumour Prognostic Studies (REMARK) guidelines 16. Eight criteria were evaluated, each rated as either adequate (1) or inadequate (0): clearly defined inclusion and exclusion criteria, study type (prospective or retrospective), patient characteristics, tumour characteristics, definition of margin status, study endpoints, follow-up duration, and identification of patients lost to follow-up. Each study was assigned a total score from 0 to 8, with a score > 5 considered as globally adequate.
Statistical analysis
We used a random-effect meta-analysis to pool data across studies. Only studies reporting aHR were considered. Heterogeneity was assessed by visual inspection of the forest plot and I2. We did not use a funnel plot to investigate publication bias due to the small number of studies. The clinical and methodological heterogeneity precluded further statistical analyses and meta-analysis regarding LC.
Results
Literature search and study identification
A flowchart of the study selection process is shown in Figure 1. The initial search identified 950 articles from PubMed, 1644 from EMBASE, and 87 from the Cochrane Library. After applying the exclusion criteria, non-English articles and irrelevant studies were discarded. After removing duplicates, 157 full-text articles were reviewed, with 7 included for both qualitative and quantitative analysis.
Characteristics of studies included
A total of 619 patients were recruited, with individual study sample sizes ranging from 45 to 180. Seven studies reported the status of the margins as a categorical variable and used a cutoff value to dichotomise the data (Tab. I) 11,17-22. The publication period spanned 19 years, from 2005 to 2024, and the patient recruitment period was from 1979 to 2020. Mean age was 60.9 years. All studies included were retrospective (LOE IV) 16. Of the 619 patients, 105 (17%) underwent neoadjuvant chemotherapy.
All patients underwent surgery (total laryngectomy [TL], total pharyngolaryngectomy [TPL], total pharyngolaryngoesophagectomy [TPLE], TOLMS and TORS). Following guidelines and institutional policies, adjuvant radiotherapy or chemoradiotherapy has been administered due to positive margins, lymph node involvement and adverse pathological features. The average of the follow-up periods was 36.6 months. Patient and tumour characteristics of the eligible studies are listed in Table II 11,17-22.
The aHR for margin status from the eligible studies are presented in Table III.
Three studies were deemed suitable to investigate the association between margin status and DSS, while 2 studies were eligible to evaluate the association between margin status and OS and DFS.
Quality assessment
After data collection, we evaluated the risk of bias in each study, independently adhering to the reporting recommendations for tumour prognostic studies (REMARK) guidelines 16. REMARK involves 8 different domains. Each domain is considered adequate (1) or not adequate (0). These domains are:
- well-defined inclusion and exclusion criteria;
- nature of the study (prospective or retrospective);
- patient characteristics described;
- tumour characteristics described;
- margin status definition described;
- study endpoints or outcomes described;
- follow-up period described;
- patients unavailable for statistical analysis identified (i.e., lost to follow-up).
We gave each study a total score from 0 to 8, indicating the lowest and highest quality, respectively. A total score > 5 was considered globally adequate. The quality of the studies ranged from 5 to 8. The median score was 6.6.
Meta-analysis results
The meta-analysis results did not provide evidence of a significant impact of margin status (positive versus negative) on OS, DSS or DFS. Using the random-effects RELM model, the analysis for OS yielded an HR of 1.78 (95%CI: 0.79-4.04) with an I2 value of 0% (p = 0.17) (Fig. 2). For DFS the HR was 1.43 (95%CI: 0.82-2.49), with an I2 of 0% (p = 0.21) (Fig. 3), while for DSS the HR was 1.31 (95%CI: 0.42-4.05), with an I2 of 86% (p = 0.42) (Fig. 4).
Discussion
Hypopharyngeal squamous cell carcinomas represent a particularly complex entity within head and neck oncology. Their aggressiveness, frequent presentation at advanced stages and the anatomical intricacies of the hypopharynx make their management highly challenging, both oncologically and functionally 9. In addition to their generally poor prognosis, these tumours exhibit a strong tendency for locoregional recurrence and distant metastasis, both of which contribute significantly to their high rate of mortality. The difficulty in achieving proper resection margins, due to the anatomical complexity of the region and the tumour’s infiltrative growth pattern, further complicates local disease control when surgery is the primary therapeutic approach 5.
In recent years, the focus on laryngeal preservation has gained prominence in the treatment of early- and intermediate-stage hypopharyngeal cancers. Non-surgical strategies such as radiotherapy or chemoradiotherapy have demonstrated oncological outcomes comparable to radical surgery, while reducing treatment-related morbidity and improving post-therapeutic quality of life 23. Simultaneously, advances in minimally-invasive surgical techniques, including TOLMS 22 and TORS 21, have expanded therapeutic options for selected cases, particularly in early-stage disease. However, in locally advanced tumours, radical surgery, typically TPL or TPLE, remains the standard treatment, whether as a primary or salvage setting, and is often combined with adjuvant therapies 11.
A major concern following surgery is the presence of positive margins, as they constitute a negative prognostic factor for local control in hypopharyngeal carcinoma. According to the RCP 7, margins are classified as free (> 5 mm), close (1-5 mm), or positive (< 1 mm). Although free and wide margins are the ideal goal, the anatomical constraints of the region and the biological behaviour of these tumours frequently make achieving margins of 5 mm or greater unfeasible 8. Close margins (1-5 mm) are generally considered acceptable and do not appear to significantly affect OS or DFS, while positive margins (< 1 mm) should be avoided due to their potential negative impact on LC and prognosis. Patients with positive margins typically require adjuvant therapies, such as (chemo)radiotherapy, yet they continue to face a high risk of local and locoregional recurrence 24.
The extensive submucosal spread of hypopharyngeal carcinoma, which often exceeds 8 mm, and the presence of skip lesions, further complicate the achievement of clear and safe margins 5. These patterns of tumour spread are difficult to detect, even with advanced imaging modalities such as magnetic resonance imaging (MRI) and narrow-band imaging (NBI) endoscopy. The variability in positive margin rates reported in the literature, ranging from 5% to 60%, reflects discrepancies in margin assessment methodologies, surgical techniques and patient selection criteria. Our review identified a mean positive margin rate of approximately 25%, regardless of the surgical approach used. For example, Tran Ann Bich in 2022 reported a 5.1% positive margins rate following highly demolitive procedures such as TPLE with gastric pull-up 19, whereas Kutter in 2007 observed a 60% incidence after TOLMS 22.
Mazerolle, in a series of 57 piriform sinus carcinomas treated primarily with TORS, reported a positive/close margin rate of approximately 30%, despite systematic intraoperative re-excisions based on clinical assessments or frozen section analysis 21. Similarly, Bova et al., in a cohort of 180 hypopharyngeal carcinomas treated with TPL, found positive margins in 11%, close margins in 9%, and negative margins in 77% of cases 20. Bernard et al. reported a 57% positive margins rate in patients undergoing TPL for advanced tumours, highlighting the significant impact of tumour size, anatomical constraints, and selection of surgical technique on oncological outcomes 8.
Despite these findings, our systematic review suggests that oncological outcomes remain satisfactory even in series with high rates of positive or close margins. This trend is particularly evident in transoral surgery series, where the rate of positive margins may be artificially elevated due to laser-induced tissue shrinkage and traction artifacts during excision in a confined space, which can complicate assessment of pathological margins 21,22. Moreover, the frequent use of adjuvant therapies, necessitated by the high rate of adverse pathological factors, may mitigate the negative impact of positive margins on LC. Additionally, many recurrences classified as local may represent locoregional recurrences occurring at the junction of the primary tumour and nodal basin.
Histopathological evaluation of surgical margins serves as an essential quality control measure for assessing the adequacy of resection. A standardised approach to specimen handling and interpretation is critical, with particular attention to technical aspects such as tissue shrinkage, sampling methodologies and fixation protocols. Sampling errors during specimen processing, especially when frozen sections are used, may lead to misinterpretation of margin status, although this technique remains a valuable tool to optimise radical resection. Bernard proposed an intraoperative macroscopic assessment of the specimen through a joint analysis by the surgeon and pathologist, including direct palpation and perpendicular incisions to the resection plane, to identify high-risk areas and guide further re-excisions 8. However, tissue contraction, thermal damage from electrosurgical instruments and sampling errors remain substantial challenges in defining surgical margins with precision.
The phenomenon of tissue shrinkage following oncological resections in head and neck tumours, along with the reduction in margin size due to the intrinsic elastic properties of tissues and formalin fixation effects, have been well documented 25. To avoid underestimation of resection margins, it is recommended that measurements be taken immediately after resection or during intraoperative assessment. Additionally, meticulous documentation of margin measurements by both surgeons and pathologists is crucial to ensure accurate interpretation.
The relationship between resection margins and oncological outcomes, including OS, DFS and LC, remains controversial. While positive margins are clearly associated with an increased risk of local recurrence, their impact on OS is less evident. Published studies have not demonstrated a significant association between free margins (> 5 mm) and OS (p = 0.286) or DFS (p = 0.11). Similarly, resection margins do not appear to be independent predictors of DSS or recurrence in either uni- or multivariate analyses. Close margins (1-5 mm) appear to be acceptable in many subsites without significantly compromising oncological outcomes, whereas positive margins (< 1 mm) should be avoided due to their detrimental effect on prognosis.
Our meta-analysis did not provide evidence of a significant impact of margin status (positive vs. negative) on OS, DSS, or DFS. Using the random-effects RELM model, we obtained an HR of 1.78 (95%CI: 0.79-4.04, I2 = 0%, p = 0.17) for OS; an HR of 1.43 (95%CI: 0.82-2.49, I2 = 0%, p = 0.21) for DFS; and an HR of 1.31 (95%CI: 0.42-4.05, I2 = 85.58%, p = 0.42) for DSS.
Our systematic review highlights the scarcity of studies investigating the clinical significance of resection margins in hypopharyngeal cancer surgery and remains inconclusive regarding their true impact on local and locoregional disease control. This analysis reinforces the necessity of a multidisciplinary and personalised approach to optimising management of hypopharyngeal carcinoma. Close collaboration among surgeons, oncologists, radiation therapists, radiologists and pathologists, combined with the integration of advanced imaging and endoscopic techniques for follow-up, can significantly improve clinical outcomes. Additionally, standardising definitions of margins and developing treatment protocols based on robust scientific evidence are essential steps in moving forward. Margins of 4-5 mm may be considered sufficiently safe, whereas close margins require careful planning of adjuvant therapies to minimise the risk of recurrence.
Conclusions
The management of hypopharyngeal carcinomas remains one of the most complex challenges in head and neck oncology. Achieving adequate resection margins is often hindered by tumour submucosal spread, anatomical constraints and surgical limitations. While free margins (> 5 mm) are ideal, close margins (1-5 mm) are generally acceptable without significantly impacting survival, whereas positive margins (< 1 mm) should be avoided due to their negative prognostic implications.
Innovative techniques such as TOLMS and TORS offer promising alternatives for early- and intermediate-stage tumours, balancing oncological control with better functional outcomes. However, for locally-advanced cases, radical surgery combined with adjuvant therapy remains the standard of care. Intraoperative collaboration between surgeons and pathologists, along with standardised margin assessment protocols, can enhance surgical precision and reduce errors.
Advancing diagnostic and therapeutic strategies is essential to addressing submucosal tumour spread and skip lesions. Integrating advanced imaging techniques, such as MRI and NBI, can improve surgical planning and LC. Additionally, standardising definitions of margins and resection criteria will help ensure consistency in oncological outcomes. A multidisciplinary and personalised approach remains key to optimize treatment outcomes and improve both survival and quality of life. Future advancements should focus on refining therapeutic strategies to better align with individual patient needs.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
FM: conception and design of the study, writing and editing the manuscript; GS: conception and design of the study, writing and editing the manuscript; FP: data collection; CG: data collection; SS: data collection; CDG: statistical analysis; AG: conception and design of the study, reviewing the manuscript; GM: reviewing the manuscript; EC: conception and design of the study, writing and editing the manuscript.
Ethical consideration
Not applicable.
History
Received: February 23, 2025
Accepted: March 31, 2025
Figures and tables
Figure 1. PRISMA flow diagram.
Figure 2. Overall survival, forest plot.
Figure 3. Disease-free survival, forest plot.
Figure 4. Disease-specific survival, forest plot.
| Study | Year | Country | Study period | Type of study | End-points | Follow-up (months) |
|---|---|---|---|---|---|---|
| Omura 17 | 2014 | Japan | 1995-2011 | Retrospective | OS, DSS | 46 |
| Grasl 18 | 2022 | Austria | 1993-2020 | Retrospective | DSS, DFS | 49.1 ± 59.6 |
| Bich 19 | 2022 | Vietnam | 2012-2016 | Retrospective | OS, DFS | 30.1 ± 23.4 |
| Bova 20 | 2005 | Australia | 1979-2002 | Retrospective | DSS | 24-60 |
| Mazerolle 21 | 2018 | France | 2009-2017 | Retrospective | OS, DFS | 23 |
| Bernard 11 | 2024 | Netherlands | 2008-2017 | Retrospective | DSS, DFS, LC | 60 |
| Kutter 22 | 2007 | Switzerland | 1999-2004 | Retrospective | LC, OS | 24 |
| OS: overall survival; LC: local control; DFS: disease-free survival; DSS: disease-specific survival. | ||||||
| Study | No. patients (male/female ratio) | Mean age (range) or standard deviation | Previous treatment | Surgery of T | Surgery of N | TNM stage |
|---|---|---|---|---|---|---|
| Omura 17 | 119 (113M/6F) | 62 (36-81) | No | TPL | ND | T2 13 (11%)T3 57 (48%T4a 49 (59%)N0 26 (22%)N1 12 (10%)N2 78 (65%)N3 3 (3%) |
| Grasl 18 | 113 (196M/17F) | 57.1 ± 9.3 | No | TL 111 (98%)TPL 2 (2%) | ND 93 (82%) | T1 8 (7.1%)T2 18 (15.9%)T3 23 (33.6%)T4a 46 (43.4%)N0 29 (25.7%)N1 13 (11.5%)N2 55 (48.7%)N3 6 (5.3%)Nx 10 (8.8%) |
| Bich 19 | 50 (47M/3F) | 60.3 (37-76) | No | TPL with gastric pull-up | ND 48 (96%) | T3N0M0 1 (2%)T4N0M0 6 (12%)T4N1M0 15 (25%)T4N2M0 25 (50%)T4N3M0 3 (6%) |
| Bova 20 | 180 (162M/18F) | 62 (29-85) | CT 82 (45.6%) | TPL | Bilateral RND 122 (67.8%)Bilateral/ipsilateral SND 14 (7.8%) | T1 11 (3.1%)T2 45 (25%)T3 63 (35%)T4 59 (32.8%)N0 53 (29.4%)N1 44 (24.4%)N2 69 (38.3%)N3 12 (6.7%) |
| Mazerolle 21 | 57 (52M/5F) | 60 (56-62) | No | TORS | ND 41 (71.9%) | T1N0 18 T1N1 3T1N2b 8T1 tot 29 (51%)T2N0 12 T2N1 5 T2N2a1 T2N2b 9T2 tot 27(47%)T3N0 1T3 tot 1 (2%) |
| Bernard 11 | 45 (35M/10F) | 65 | No | TPL 36 (80%)TL 9 (20%) | ND | pT1 and pT2 5(11.1%)pT3 and pT4 40(88.9%)pN0 25(55.6%) |
| Kutter 22 | 55 (35M/20F) | 60 (46-87) | No | TOLMS | ND 43 (78.2%) | Stage I 15 (27%)Stage II 12 (22%)Stage III 11 (20%)Stage IV 17 (31%) |
| TPL: total pharyngolaryngectomy; TPLE: total pharyngolaryngo-esophagectomy; TL: total laryngectomy; ND: neck dissection; RND: radical neck dissection; TOLMS: transoral laser microsurgery; TORS: transoral robotic surgery; RT: radiotherapy; CT: chemotherapy. | ||||||
| Study | Margins | Adjuvant treatment | Oncological results | Ahr value |
|---|---|---|---|---|
| Kutter 22 | Negative margin 17/55 (30.9%)Close or positive margin 33/55 (60%) | RT 18/55 (38%)TOLMS15/55(29%) | OSNegative margin 79%Close or positive margin 75%LCNegative margin 91%Close or positive margin 88%2y DFSNegative margin 59%Close or positive margin 75% | p 0.25p 0.38p 0.84 |
| Bernard 11 | Negative margin 12%Close margin (< 5 mm) 31%Positive margin (< 1 mm) 57% | RT 29/45 (64%) | LCNegative margin 33%Close margin 7%Positive margin 18%5y DSSNegative margin 67%Close margin 70%Positive margin 40%5y DFSNegative margin 33%Close margin 50%Positive margin 18% | p 0.942p 0.207p 0.030 |
| Mazerolle 21 | Negative margin 40/57 (70%) | RT 12/57 (21%)TPL 2/57 (3.5%)CT+RT 17/57 (30%) | OS84% at 24 months66% at 48 monthsDSF74% at 24 months50% at 48 months | - |
| Bova 20 | Positive margin 19/180 (11%)Close margin (< 5 mm) 16/180 (9%)Negative margin 139/180 (77%) | RT 169/180 (94%) | DSSR0 vs positive HR = 0.54 (95%CI, 0.32-0.91) | p 0.02 |
| Bich 19 | Negative margin 47Positive margin 3 | RT 46 (92%) | OSR0 vs R1, HR 1.23 (95%CI, 0.29-5.27)DFSR0 vs R1 HR 1.19, (95%CI, 0.28-5.10) | p 0.776p 0.812 |
| Omura 17 | Positive margin 7/119 (5.9%)Negative margin 112/119 (94%) | RT/CT 26/119 (22%) | Univariate DSSR1 vs R0 4.80 (95%CI, 1.17-19.8)Multivariate DSSR0 vs R1 2.35 (95%CI, 0.86-6.40)Multivariate OSR0 vs R1 2.12 (95%CI, 0.79-5.71) | p 0.03p 0.09p 0.14 |
| Grasl 18 | Negative margin 95 (84.1%)Close margin 16 (14.2%)Positive margin 2 (1.8%) | RT 70 (61.9%) | 1y – DSSPositive margin 77.8%Negative margin 85%3y – DSSPositive margin 44.9%Negative margin 59.4%5y – DSSPositive margin 44.9%Negative margin 50%DSS R0 vs R1 0.75 (95%CI, 0.41-1.38)1y – DFSPositive margin 50%Negative margin 75%3y – DFSPositive margin 45%Negative margin 56%5y – DFSPositive margin 45%Negative margin 51%DFS R0 vs R1 0.68 (95%CI, 0.37-1.24) | p 0.357p 0.210 |
| RT: radiotherapy; TOLMS: transoral laser microsurgery; OS: overall survival; LC: local control; DFS: disease-free survival; DSS: disease-specific survival. | ||||
References
- Bradley P. Symptoms and signs, staging and co-morbidity of hypopharyngeal cancer. Adv Otorhinolaryngol. 2019;83:15-26. doi:https://doi.org/10.1159/000492304
- Aupérin A. Epidemiology of head and neck cancers: an update. Curr Opin Oncol. 2020;32:178-186. doi:https://doi.org/10.1097/CCO.0000000000000629
- Eckel H, Bradley P. Future perspectives in hypopharyngeal cancer care. Adv Otorhinolaryngol. 2019;83:167-175. doi:https://doi.org/10.1159/000492361
- Saito Y, Omura G, Yasuhara K. Prognostic value of lymphovascular invasion of the primary tumor in hypopharyngeal carcinoma after total laryngopharyngectomy. Head Neck. 2017;39:1535-1543. doi:https://doi.org/10.1002/hed.24705
- Zbären P, Egger C. Growth patterns of piriform sinus carcinomas. Laryngoscope. 1997;107:511-518. doi:https://doi.org/10.1097/00005537-199704000-00015
- Piazza C, Paderno A, Ravanelli M. Clinical and radiological evaluation of hypopharyngeal carcinoma. Adv Otorhinolaryngol. 2019;83:35-46. doi:https://doi.org/10.1159/000492306
- Helliwell T. The Royal College of Pathology. Standards and datasets for reporting cancers. Dataset for histopathology reporting of mucosal malignancies of the larynx. Published online 2013.
- Bernard S, van Lanschot C, Hardillo J. A new proposal for adequate resection margins in larynx and hypopharynx tumor surgery – Are the RCP Guidelines feasible?. Cancers (Basel). 2024;16. doi:https://doi.org/10.3390/cancers16112058
- Helliwell T. Best practice no 169. Evidence based pathology: squamous carcinoma of the hypopharynx. J Clin Pathol. 2003;56:81-85. doi:https://doi.org/10.1136/jcp.56.2.81
- Nishimura A, Yokota T, Hamauchi S. Prognostic impact of the number of metastatic lymph nodes after surgery in locally advanced hypopharyngeal cancer. BMC Cancer. 2022;22. doi:https://doi.org/10.1186/s12885-022-10172-8
- Bernard S, van Lanschot C, Sewnaik A. Clinical relevance of resection margins in patients with total laryngectomy or laryngopharyngectomy. Cancers (Basel). 2024;16. doi:https://doi.org/10.3390/cancers16112038
- Saraniti C, Speciale R, Gallina S. Prognostic role of resection margin in open oncologic laryngeal surgery: survival analysis of a cohort of 139 patients affected by squamous cell carcinoma. Braz J Otorhinolaryngol. 2019;85:603-610. doi:https://doi.org/10.1016/j.bjorl.2018.04.012
- McInnes M, Moher D, Thombs B. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319:388-396. doi:https://doi.org/10.1001/jama.20017.19163
- Lydiatt W, Patel S, O’Sullivan B. Head and neck cancers – Major changes in the American Joint Committee on Cancer Eight Edition Cancer Staging Manual. CA Cancer J Clin. 2017;67:122-137. doi:https://doi.org/10.3322/caac.21389
- Tucker S, McNett M, Mazurek Melnyk B. Implementation science: application of evidence-based practice models to improve healthcare quality. Worldviews Evid Based Nurs. 2021;18:76-84. doi:https://doi.org/10.1111/wvn.12495
- Altman D, McShane L, Sauerbrei W. Reporting recommendations for tumor marker prognostic studies (REMARK): explanation and elaboration. PLoS Med. 2012;9. doi:https://doi.org/10.1371/journal.pmed.1001216
- Omura G, Ando M, Saito Y. Disease control and clinicopathological prognostic factors of total pharyngolaryngectomy for hypopharyngeal cancer: a single-center study. Int J Clin Oncol. 2015;20:290-297. doi:https://doi.org/10.1007/s10147-014-0709-z
- Grasl S, Frommlet F, Faisal M. A new nomogram to predict oncological outcome in laryngeal and hypopharyngeal carcinoma patients after laryngopharyngectomy. Eur Arch Otorhinolaryngol. 2023;280:1381-1390. doi:https://doi.org/10.1007/s00405-022-07668-1
- Bich T, Vuong N, Cam Tu N. Long-term survival of patients after total pharyngolaryngoesophagectomy with gastric pull-up reconstruction for hypopharyngeal or laryngeal cancer invading cervical esophagus. Ann Otol Rhinol Laryngol. 2023;132:511-518. doi:https://doi.org/10.1177/00034894221098802
- Bova R, Goh R, Poulson M. Total pharyngolaryngectomy for squamous cell carcinoma of the hypopharynx: a review. Laryngoscope. 2005;115:864-869. doi:https://doi.org/10.1097/01.MLG.0000158348.38763.5D
- Mazerolle P, Philouze P, Garrel R. Oncological and functional outcomes of trans-oral robotic surgery for pyriform sinus carcinoma: a French GETTEC group study. Oral Oncol. 2018;86:165-170. doi:https://doi.org/10.1016/j.oraloncology.2018.09.014
- Kutter J, Lang F, Monnier P. Transoral laser surgery for pharyngeal and pharyngolaryngeal carcinomas. Arch Otolaryngol Head Neck Surg. 2007;133:139-144. doi:https://doi.org/10.1001/archotol.133.2.139
- Lefebvre J, Chevalier D, Luboinski B. Larynx preservation in pyriform sinus cancer: preliminary results of a European Organization for Research and Treatment of Cancer phase III trial. J Natl Cancer Inst. 1996;88:890-899. doi:https://doi.org/10.1093/jnci/88.13.890
- Rodrigues J, Breda E, Monteiro E. Surgically-treated locoregionally advanced hypopharyngeal cancer: outcomes. Int Arch Otorhinolaryngol. 2018;22:443-448. doi:https://doi.org/10.1055/s-0038-1641562
- Umstattd L, Mills J, Critchlow W. Shrinkage in oral squamous cell carcinoma: an analysis of tumor and margin measurements in vivo, post-resection, and post-formalin fixation. Am J Otolaryngol. 2017;38:660-662. doi:https://doi.org/10.1016/j.amjoto.2017.08.011
Downloads
License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Copyright
Copyright (c) 2025 Società Italiana di Otorinolaringoiatria e chirurgia cervico facciale
How to Cite
- Abstract viewed - 1642 times
- PDF downloaded - 426 times



